Emergent Delivery of Infant
The management of the female who presents to the emergency department (ED) in active labor is stressful and overwhelming. Ideally, the ED has a plan in place, based on hospital resources, for the imminent delivery of a newborn. Decisions regarding delivery in the ED or transferring the patient to labor and delivery are based on a variety of factors. Knowledge of the possible complications of delivery will provide anticipatory guidance to improve maternal and fetal outcomes. See Table 1 for important components of assessing and managing the pregnant patient.1,2
|
Table 1. Assessment of Pregnant Patient in the ED |
|---|
|
History |
|
|
Physical Exam |
|---|
|
Maternal complications during the peripartum period include placenta previa, placental abruption, cord prolapse, pre-eclampsia, eclampsia, and HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome. Supportive therapy and urgent referral for delivery of the infant may be required.
The presence of placenta previa is a contraindication to a digital or speculum examination. Emergency cesarean section may be required, and urgent obstetric referral is warranted. Placental abruption, which has an incidence of 1% of all pregnancies, may be due to trauma, drug use, advanced maternal age, or smoking. The patient may present with abdominal pain and vaginal bleeding. Intravenous access, CBC, coagulation studies, and urgent obstetric consultation are required. Pre-eclampsia is hypertension with a blood pressure > 140/90, with proteinuria, and with or without peripheral edema. The patient may complain of headaches, abdominal pain, and extremity swelling. Eclampsia is the presence of seizures in a patient with hypertension or pre-eclampsia. The treatment of severe pre-eclampsia and eclampsia involves administration of magnesium sulfate 4-6 g over 15 minutes and then 1-2 g per hour, antihypertensive medications, and delivery of the infant.3 Factors that increase the risk of neonatal complications include prematurity, multiple fetuses, and abnormal presentations such as breech, shoulder, or cord. Specific neonatal complications, such as respiratory distress syndrome and meconium aspiration, are discussed in the section on neonatal resuscitation.
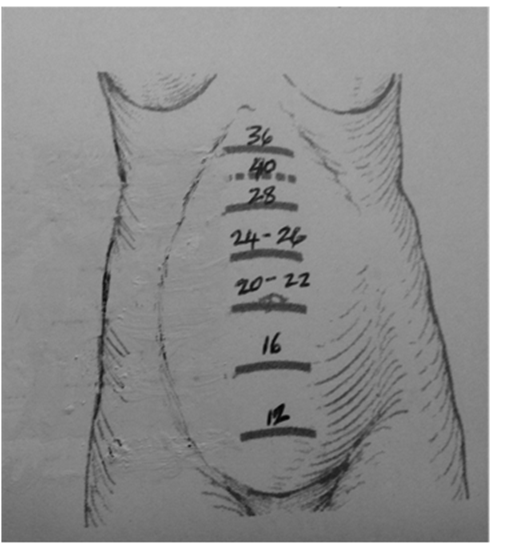
The palpation of the abdomen may help in assessing the position and presentation of the fetus. An abnormal presentation may be confirmed by a quick bedside ultrasound, if available. Fundal height also may be used to approximate gestational age. (See Figure: Approximate Gestational Age Based on Fundal Height) The presence of multiple gestation also can be ascertained by ultrasound.
Figure. Approximate Gestational Age Based on Fundal Height
Pelvic examination is important to determine whether the membranes are intact and if meconium is present. Vaginal bleeding is a contraindication to pelvic exam and should prompt an ultrasound evaluation to exclude placenta previa. Speculum or digital examination is contraindicated in the presence of vaginal bleeding. If there is no vaginal bleeding and rupture of membranes (ROM) is suspected, the patient should be evaluated with a sterile speculum, and a nitrazine test should be done to confirm ROM. Amniotic fluid turns the yellow strip dark blue. Lubricant may produce a false-positive nitrazine test and its use should be avoided. Digital examination increases the risk of infection with ROM and should be avoided if possible.
Digital examination is important to assess the dilatation, station, and effacement of the cervix and to determine fetal presentation (occiput, breech, shoulder, face, brow, compound, or cord). The station indicates the position of the presenting part of the fetus in the pelvis. The maternal ischial spines are the reference point for assessing the station. A negative station refers to the presenting part lying above the spines, 0 station at level of the ischial spines, and +1, +2, +3 below the spines; the latter is consistent with the scalp being visible at the introitus.
Stages of Labor
The first stage of labor is the onset of contractions to the complete dilation of the cervix (10 cm). The duration of labor varies with factors such as size of pelvis, size of fetus, and parity. The duration of the first stage of labor in the primiparous patient ranges from 6-18 hours and from 2-10 hours in the multiparous patient.4
ROM is timely if it occurs at the end of the first stage of labor. It is premature if it occurs before labor begins. Early ROM occurs with rupture before cervical dilation to 6 cm is achieved.3
The second stage of labor is the period between complete dilatation of the cervix and delivery of the newborn. Contractions occur every 2-3 minutes and last about 1 minute. The second stage varies with the parity of the mother. The median duration of the second stage is about 50 minutes in the primiparous patient (about 20 pushes) and 20 minutes (a few pushes) in the multiparous patient.4,5
The third stage of labor is the period between the birth of the newborn and the expulsion of the placenta. The duration is about 10-30 minutes.
Management
The decision to deliver an infant in the ED is determined by several factors, including the stage of labor, the parity of the pregnant patient, and the proximity to labor and delivery/obstetrical services.
True labor must be distinguished from false labor. False labor is represented by Braxton Hicks contractions, usually in the lower abdomen, which are brief, irregular, and ineffective in producing changes in the cervix.
If the patient has the urge to push or defecate, the second stage of labor should be suspected. Contractions occur at regular intervals, with abdominal or back pain, and are associated with dilation and effacement of the cervix.3,6
The assignment of tasks to the team caring for the mother and the team caring for the infant is important prior to the delivery. Equipment needed for an emergency delivery includes sterile gloves, sterile towels and drapes, surgical scissors, hemostats, cord clamps, gauze sponges, syringes, needles, suction bulb, placenta basin, and supplies for resuscitation of the neonate. A radiant warmer or incubator should be available to keep the infant warm. The neonatal and obstetrical team, if available, should be alerted and present as soon as possible to help in the care of the infant and the mother, respectively.
Supplemental oxygen and intravenous fluids should be administered to the mother if fetal distress is suspected. Lateral positioning is recommended to prevent compression of the vena cava, which can occur in the supine position. This can produce maternal hypotension and decreased blood flow to the fetus.
When considering transport of a pregnant patient to labor and delivery, the following factors must be considered: the stage of labor, the parity of the patient, the transit time to an intramural or extramural facility, and availability of qualified transport personnel. Obstetric consultation should be obtained as early as possible.
The pregnant patient must be examined and deemed stable for transfer to a facility with obstetric facilities or labor and delivery. Informed consent is necessary prior to transfer. An appropriate transfer is one in which the transferring facility provides care within its capacity, while minimizing the risks to the patient’s health and the unborn child. The receiving facility must have an available bed and qualified personnel, and must agree to take the transfer. See Emergency Medical Treatment and Labor Act (EMTALA) for specific guidance.5,7
A woman in active labor with painful contractions has an emergent medical condition. If there is insufficient time for transfer before delivery or if the transfer poses a risk to the health or safety of the fetus, this patient, per EMTALA, may not be transferred from the ED.
A multiparous patient in the second stage of labor likely will need to be delivered in the ED. A cervix that is fully dilated and effaced, or the presence of the infant’s head in the vagina, suggests that delivery will occur within minutes, so transferring to labor and delivery is not recommended.
The pregnant patient is encouraged to take slow deep breaths, and oxygen may be administered to maximize oxygenation of the fetus. The second stage of labor has the highest risk for hypoxia. Intravenous access is recommended.
The dorsal lithotomy position is the usual position for delivery of the infant. The perineum may be cleansed with betadine if time permits. The area should be draped. A sterile towel is placed over the lower part of the perineum. The medical personnel should be appropriately attired.
The perineum is protected by controlled gradual delivery of the head; the back of the head is supported with the left hand and the right hand guides the head from the perineum. The mouth and nose should be suctioned as soon as the head is delivered. The perineum stretches as the newborn passes through. If cord prolapse is discovered during the bimanual examination, the hand should remain in the vagina to elevate the presenting fetal part to prevent cord compression while being transported to the operating room for an emergency cesarean section.
Episiotomy is not routinely recommended. The head should be lowered to facilitate the birth of the shoulders, with gentle traction. The infant’s body is lifted over the symphysis onto the mother’s abdomen. One should check for a nuchal cord and loosen if necessary, prior to delivering the infant. The umbilical cord is clamped in two places about 4-5 cm from the infant’s abdomen. The cord is then cut between the two clamps. A plastic clamp is then placed 2-3 cm from the infant’s abdomen. Document the exact time of arrival of the infant. The infant is dried and stimulated and kept warm under a radiant warmer or on the mother’s abdomen.1,3,4 The infant is examined to assess the condition after birth and the need for resuscitation.8 (See section on resuscitation for more specific details.)
The third stage of labor occurs between the delivery of the infant and the expulsion of the placenta by the uterus. Gently remove the placenta after separation to prevent ripping and retained products of conception. Examine the placenta to make sure that it is complete. The massage of the uterus is performed to promote contractions and reduce bleeding. Observe the patient carefully for excess uterine bleeding. Oxytocin (10-20 units in normal saline intravenously or 10 units intramuscularly) may be administered to prevent hemorrhage after delivery by promoting uterine contractions.
RhoGAM 300 mcg IM should be administered to the Rh-negative mother with an RH-positive infant within 72 hours of delivery.9 The infant should receive ophthalmic prophylaxis with erythromycin ointment 0.5% and vitamin K (0.5 mg to 1 mg) IM within 1 hour of delivery.8,9
Breech Presentation
Breech presentation occurs in 3-4% of term pregnancies and is associated with increased morbidity and mortality. Complications include entrapment of the head and cord prolapse. Urgent obstetric consultation is necessary for breech presentations. Frank or complete breech may dilate the cervix as a cephalic presentation, so the delivery may proceed without complications. Avoid handling the fetus until the cord is visible. The fingers of the examiner should be placed medial to each thigh and the thigh pushed out laterally to deliver the legs. Rotate the fetus to a position with the sacrum anterior. When the scapula is visible, gently rotate until the right arm is delivered, then rotate counter-clockwise until the other arm is delivered. The examiner should then place the middle and index finger over the lower jaw of the fetus to keep the head flexed and assist the delivery of the infant. The footling or incomplete breech is unsafe for vaginal delivery, and every effort should be made to obtain the expertise of an obstetrician.3
Shoulder Dystocia
Complications of shoulder dystocia include brachial plexus injury and hypoxia. If the shoulder is impacted, the mother should be placed in the extreme lithotomy position, the bladder drained, and suprapubic pressure applied. An episiotomy is recommended to facilitate the delivery. Grasping the posterior scapula and rotating the shoulder girdle 180 degrees in the pelvic outlet may deliver the shoulder (Wood’s maneuver). If this is unsuccessful, the examiner may place his hand in the vagina to grasp the posterior arm. The elbow is flexed and the arm and posterior shoulder are delivered, followed by the anterior shoulder.3
Multiple Fetuses
The presence of more than one fetus requires additional delivery kits and staff to deliver and care for the infants.
Cesarean Section for Maternal Cardiac Arrest
In cases of maternal cardiac arrest with a viable fetus, a perimortem emergency cesarean section is warranted. If performed within 5 minutes of maternal arrest, the prognosis for the infant is good. The ED physician may be required to perform this procedure in the absence of a more qualified individual, such as an obstetrician or surgeon.
Maternal CPR should be performed before and throughout the cesarean section.10,11,12 It is not necessary to check for fetal viability prior to the procedure.
A classic midline incision is made about 5 cm below the xiphoid process to the pubic symphysis. Blunt dissection of the rectus muscle and then incision of the peritoneum is performed to expose the uterus. An incision is made in the uterus from the fundus to where the bladder adheres to the uterus. The fetus is removed and resuscitated. The placenta is removed and the uterus is repaired with chromic 0 or 1 running suture. The skin of the abdominal wall is then closed. The infant should be transferred to a neonatal unit after resuscitation and stabilization.
Emergent Delivery References
-
Hansmann G. Neonatal Emergencies. A Practical Guide for Resuscitation, Transport and Critical Care of Newborn Infants. Cambridge University Press; 2009:
249-256. - Benson R. Handbook of Obstetrics and Gynecology. 8th ed. Los Altos, CA: Lange Medical Publications; p 65.
- VanRooyen M, Fortner K. Emergency Delivery. In: Emergency Medicine. A Comprehensive Study Guide. Tintinalli JE, Kelen GD, Stapczynski JS, eds. American College of Emergency Physicians. 2004: 684-691.
- Benzoni TE. Labor and Delivery in the Emergency Department Clinical Presentation. Medscape. Available at: http://emedicine.medscape.com/article/796379-clinical. Accessed November 15, 2014.
- Cunningham F, Leveno K, Bloom S, et al. Williams Obstetrics. 23rd ed. New York: McGraw Hill; 2010: 141-146.
- Centers for Medicare & Medicaid Services. Emergency Medical Treatment & Labor Act (EMTALA). Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/EMTALA/Index.html/EMTALA/. Accessed: November 15, 2014.
- Social Security Administration. Examination and Treatment for Emergency Medical Conditions and Women in Labor. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1867.htm#t. Accessed November 15, 2014.
- Kattwinkel J, Perlman JM, Aziz K, et al. Neonatal Resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular and Emergency Cardiovascular Care. Pediatrics 2010;126:e1400-1413.
- American Academy of Pediatrics. The American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 4th ed. Pp. 151,157.
- Datner E, Promes S. Resuscitation Issues in Pregnancy. In: Emergency Medicine. A Comprehensive Study Guide. Tintinalli JE, Kelen GD, Stapczynski JS, eds. American College of Emergency Physicians; 2004: 98-99.
- Katz V, Balderston K, DeFreest M. Perimortem cesarean delivery: Were our assumptions correct? Am J Obstet Gynecol 2005;192:1916-1921.
- 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: Part 10.8: Cardiac Arrest Associated With Pregnancy. Ciculation 2005; 112:IV-150-153, published online before print November 28, 2005, doi: 10.1161/CIRCULATIONAHA.105.166570.
