Congenital Anomalies: HEENT Emergencies
Core Content: Emergency Management of Congenital Anomalies
- Know the anatomy and pathophysiology relevant to emergency management of congenital anomalies
- Know the indications and contraindications for emergency management of congenital anomalies
- Plan the key steps and know the potential pitfalls in the emergency management of congenital anomalies
- Recognize the complications associated with the emergency management of congenital anomalies
HEENT EMERGENCIES
Caput Succedaneum. Caput succedaneum is swelling of the scalp above the periosteum due to the pressure of the cervix and vaginal walls on the head during vaginal delivery. Unlike cephalhematomas, it may cross suture lines. Caput succedaneum is usually benign and resolves within in a few days without treatment.
Cephalohematoma A cephalohematoma is a collection of blood under the periosteum of the skull. It occurs in 1-2% of newborns due to birth trauma. On palpation, the swelling is fluctuant and does not cross suture lines. Cephalohematomas require no treatment but may take several weeks to resolve. Large cephalohematomas increase the risk for hyperbilirubinemia. Subgaleal Hematoma A subgaleal hematoma is a collection of blood between the periosteum of the skull and the galea aponeurosis of the scalp usually secondary to birth trauma (most commonly vacuum assisted deliveries). The swelling is diffuse and usually fluctuant, and it typically will cross suture lines and obscure the fontanelles. Because the subgaleal space is a large potential space extending from the orbital ridges to the nape of the neck, there is the potential for massive blood loss (up to 50% of a newborns total blood volume) resulting in hemorrhagic shock. Morbidity and mortality associated with subgaleal hemorrhages is significant. Treatment involves controlling hemorrhage and the neonate may require transfusions with packed red cells and fresh frozen plasma.
CME Question
A 3-day-old infant presents to the ED with scalp swelling. The birth history is significant for a term, large for gestational age infant, who had a vacuum assisted delivery. Regarding this infant, which of the following is true:
- A cephalohematoma can cause severe anemia and shock.
- A subgaleal hematoma is usually a benign condition.
- A cephalohematoma does not cross suture lines.
- A cephalohematoma occurs between the periosteum of the skull and the galea aponeurosis.
Start or Resume CME Test (Opens in a new Tab/Window)
| Caput succedaneum | Celphalohematoma | Subgaleal hematoma |
| Scalp swelling due to pressure of cervix and vaginal walls during delivery | Collection of blood under the periosteum | Collection of blood between the skull periosteum and the galea |
| Can cross suture lines | Does not cross suture lines | Can cross suture lines |
| No treatment necessary. Resolves in a few days. | No treatment necessary. Resolves in a few weeks. May increase bilirubin levels. | This may cause severe anemia from hemorrhage into the space. Blood transfusion with packed red blood cells and fresh frozen plasma may be required depending on severity of the hemorrhage. |
Craniosynostosis. The premature closure of one or more cranial sutures results in craniosynostosis and is associated with syndromes such as Apert or Crouzon. This may result in an abnormally shaped head, poor brain growth, and increased intracranial pressure. Lambdoid synostosis may be confused with positional plagiocephaly. It is best distinguished by viewing the head from the vertex. The infant’s ear in positional plagiocephaly is displaced anteriorly from the affected suture. In lambdoid synostosis, the ear is displaced posteriorly from the affected suture. Diagnosis is confirmed by CT head and skull X-rays. Neurosurgical consultation is mandatory for craniosynostosis.
CME Question
A 1-month-old infant presents with an abnormally shaped head. The parents are very concerned. You suspect craniosynostosis. Which of the following statements is true regarding this condition?
- A.A CT of the head and skull X-rays are helpful for the diagnosis.
- B.Poor head control and sun-setting eyes may occur.
- C.Neurosurgical consultation is recommended.
- D.There is an association with Apert’s syndrome and Crouzon’s syndrome.
- E.All of the above.
Start or Resume CME Test (Opens in a new Tab/Window)
Hydrocephalus. Hydrocephalus is the accumulation of excess cerebrospinal fluid (CSF) in the ventricles of the brain, either as a result of impaired CSF circulation (obstructive or non-communicating hydrocephalus) or impaired CSF absorption (communicating hydrocephalus). In children, hydrocephalus is almost always associated with increased intracranial pressure. Risk factors include prematurity and infection. It occurs in approximately 35% of preterm infants with intraventricular hemorrhage. Clinical symptoms of hydrocephalus are secondary to increased ICP and may be vague and nonspecific, including vomiting, behavioral changes, and developmental delay or regression. Physical signs may include bradycardia (part of Cushing’s phenomenon), macrocephaly, cranial nerve palsies, papilledema, or extremity spasticity. Diagnosis is made with an ultrasound or CT of the head. (See Figure. Head CT showing hydrocephalus) Neurosurgical consultation is necessary for placement of a shunt (ventriculoperitoneal or ventriculoatrial). (See Figure. Ventriculoperitoneal Shunt in an Infant)


Once a CSF shunt has been placed, the two most common complications that may develop are malfunction and infection. Shunt malfunction may occur due to obstruction of the tubing, tube breakage, excess drainage, or migration of the tubes. In addition, newer electronically programmable shunt devices may malfunction if they are not properly reprogrammed after MRI imaging. Infants with a malfunctioning shunt may display signs and symptoms of increased intracranial pressure. Shunt series X-rays and CT of the head confirm the diagnosis. Urgent neurosurgical consultation is necessary for shunt replacement.
Shunt infection occurs in about 10% of infants with shunts and usually occurs within 6 months of the shunt placement. Organisms causing infections are often skin flora such as Staphylococcus epidermidis, Staphylococcus aureus, enteric bacteria such as Escherichia coli or diphtheroids, and Streptococcus species. The infant may present with or without fever, irritability, and meningeal signs. Neurosurgery consultation and CSF analysis establishes the diagnosis. Treatment includes removal and externalization of the infected shunt as well as intravenous antibiotics (usually vancomycin until culture results available) for at least 14 days.
CME Question
A 4-week-old infant, who has a ventriculo-peritoneal shunt, presents to the emergency department with fever, irritability and a bulging fontanel. Which of the following is true regarding this infant?
- Shunt infections typically occur greater than 6 months after placement.
- The organisms involved are usually skin flora such as staphylococcus epidermidis, staphylococcus aureus.
- The shunt should be tapped for CSF analysis prior to neurosurgical consultation.
- Fever is always present.
Start or Resume CME Test (Opens in a new Tab/Window)
Ophthalmia Neonatorum. Chlamydial conjunctivitis is the most common cause of ophthalmia neonatorum (conjunctivitis of the newborn) in the United States, with an incidence of 6.2 per 1000 live births. (See Figure: Conjunctivitis) The infant is often infected during vaginal delivery with an incubation period of 5-14 days after delivery. The infant usually presents with conjunctival injection and watery-to-mucopurulent exudate. Eyelid scarring and pannus (membrane of granulation tissue) formation is a late complication if untreated. Culture of the conjunctival epithelium of the everted eyelid is the gold standard for diagnosis. Chlamydia trachomatis is an obligate intracellular organism and the exudate is an insufficient sample for testing. Testing for gonococcal co-infection is recommended as co-infection is common. The treatment is oral erythromycin (50 mg/kg/day q6h) for 14 days. Close follow-up is important because treatment failure may occur and a second course of erythromycin may be required. Pyloric stenosis is a possible complication of macrolide therapy in the first 2 weeks of life. Infants treated should be closely monitored for this complication.
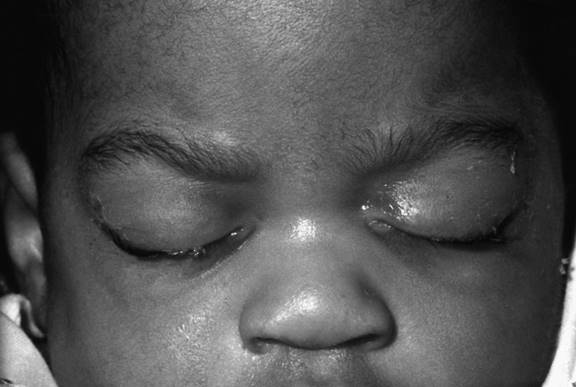
Neisseria gonorrhea often produces a severe, bilateral conjunctivitis in the newborn. It occurs usually between 2-5 days of life. The incidence in the United States is significantly decreased due to routine prophylaxis. There is often a copious purulent discharge, lid edema, and chemosis. Complications include corneal ulcers, perforation, and blindness. Diagnosis is made by gram stain for intracellular diplococci and culture on a modified Thayer-Martin culture medium. Cultures of the oropharynx and anus should be done on affected infants. Testing for concurrent chlamydial infection is also recommended. Treatment is a single dose of ceftriaxone 25-50 mg/kg (maximum 125 mg) IV or IM. Ophthalmology should be emergently consulted. The infant should be evaluated and hospitalized for disseminated disease. Herpetic conjunctivitis is rare and is often part of a disseminated infection in the newborn period. It usually occurs in the first 2 weeks of life with unilateral or bilateral conjunctival injection, nonpurulent drainage, and lid edema. Fluorescein staining shows a corneal defect; microdendrites or geographic ulcers may be present. Diagnostic evaluation should include consideration of systemic disease. Treatment is with intravenous acyclovir and emergent ophthalmology consultation. The most effective manner in which to prevent ophthalmia neonatorum is to diagnosis and treat these infections in pregnant women prior to labor and delivery. In addition, prophylactic eye antibiotic administration (erythromycin 0.5% ophthalmologic ointment) at the time of birth is effective in reducing the risk of gonococcal disease but is ineffective in preventing chlamydial infection. For women with active genital HSV lesions at the time of labor, cesarean section is recommended. National Guideline/Academic Resource http://one.aao.org/preferred-practice-pattern/conjunctivitis-ppp--2013
CME Question
A 10-day-old infant comes to the emergency department for bilateral eye redness and yellow discharge. The mother has a history of Chlamydia infection. The following is true regarding Chlamydia conjunctivitis.
- An effective treatment is erythromycin ophthalmic ointment.
- Effective treatment is oral erythromycin (50 mg/kg/day) in 4 divided doses.
- Erythromycin ophthalmic ointment used at birth is very effective for prophylaxis of chlamydia conjunctivitis.
- Culture of the exudate is the gold standard for the diagnosis of Chlamydia conjunctivitis.
Start or Resume CME Test (Opens in a new Tab/Window)
| Organism | Diagnosis | Treatment | Age of Presentation |
|---|---|---|---|
| Chlamydia trachomatis | Culture of conjunctival epithelium |
Erythromycin 12.5 mg/kg PO every 6 hours x 14 days Efficacy is 80% Must check for concurrent pneumonia and treatment failure Repeat treatment if necessary |
5-14 days |
| Neisseria gonorrhea | Culture on modified Thayer-Martin culture medium |
Ceftriaxone 25 to 50 mg/kg (max 125 mg) IV or IM single dose or cefotaxime 100 mg/kg IV or IM single dose at birth Aggressive saline eye irrigation Ophthalmology consult |
3-5 days |
| Herpes simplex virus |
Viral culture Fluorescein staining to detect corneal defects |
Acyclovir 20 mg/kg IV every 8 hours x 14 days and a topical ophthalmic agent Trifluridine 1% Ophthalmology consult |
First 2 weeks of life |
| Haemophilus influenza, Staphylococcus aureus, Streptococcus viridans, Staphylococcus epidermidis, Escherichia coli, Streptococcus pneumoniae, Moraxella catarrhalis | Eye culture |
Erythromycin or gentamicin ophthalmic ointment Topical sulfacetamide, trimethoprim-polymyxin B, or tobramycin |
First few weeks |
| Pseudomonas aeruginosa | Eye culture |
IV and topical aminoglycosides required Ophthalmology consult |
First few weeks |
Corneal Abrasion. Corneal abrasions commonly occur in neonates, usually when they scratch their eye with their fingernails. The infant may present with persistent crying, increased tearing, and conjunctival injection. Diagnosis with fluorescein staining of the eye is facilitated by application of a topical anesthetic solution followed by fluorescein. Inspection of the eye with a Wood’s lamp will reveal the epithelial defect. Treatment includes an ophthalmic ointment, such as erythromycin, and ophthalmology follow-up within approximately 24 hours.
CME Question
A 2-week-old infant is very irritable. The infant is afebrile with no respiratory symptoms. Fluorescein staining of the eyes reveals a right corneal abrasion. What is true regarding this condition?
- Persistent crying is a common presentation of a corneal abrasion in an infant.
- The corneal abrasion requires emergent ophthalmology follow up.
- The treatment is with topical ophthalmic ointment such as Erythromycin.
- All of the above.
- A and C.
Start or Resume CME Test (Opens in a new Tab/Window)
Leukocoria. Direct ophthalmoscopic examination of the infant’s eye normally reveals a red pupilary reflex, referred to as the “red reflex.” A white pupillary reflex is abnormal and is termed leukocoria, Causes of leukocoria include retinoblastoma, vitreous hemorrhage from head trauma, retinopathy of prematurity, cataracts, and intrauterine infections such as rubella and toxocariasis.
Retinoblastoma is the most common intraocular tumor of childhood, occurring in about 1 in 15,000 live births. It has hereditary and sporadic forms. The hereditary form (25%) is usually bilateral and presents in the first year of life. The sporadic form is more often unilateral and presents after the first year of life. Leukocoria and strabismus are common presenting findings. A family history of retinoblastoma or osteogenic sarcoma is associated with an increased risk for retinoblastoma. Diagnosis is suggested by calcification in the tumor on CT or ultrasound. Urgent ophthalmologist referral is indicated.
CME Question
An infant is referred from the local health department because of an abnormal white reflex, or leukocoria, in both eyes. Appropriate management of this infant include :
- You should reassure the parents that this is normal, and no further testing is necessary.
- Perform an eye examination to confirm the finding, and order CT scan or ultrasound of the orbit.
- Refer the child to genetics for evaluation.
- Neuroblastoma is the most common intraocular tumor of childhood.
Start or Resume CME Test (Opens in a new Tab/Window)
Dacryostenosis/Dacryocystitis. Up to 20% of newborns have dacryostenosis, which is an obstruction of the nasolacrimal duct. The majority of cases are due to blockage at the membrane of Hasner (near the distal end of the nasolacrimal duct). Typically neonates presents with excessive tearing with no nasal drainage. Crusting or matting of the eyelid may occur without conjunctival injection. Palpation of the lacrimal sac may cause tears and/or mucoid discharge to be expressed from the puncta.
Treatment involves massage of the duct three times a day to provide pressure to relieve the obstruction at the membrane of Hasner. It usually resolves by 6 months of age. If it persists after 12 months of age, ophthalmology referral is recommended for lacrimal duct probing.
Infection with mucopurulent drainage may occur as a complication of the duct blockage and is called dacrocystitis. The duct may be edematous, with warmth and tenderness to palpation. Dacrocystitis requires admission for intravenous antibiotics and ophthalmology consultation. Complications include periorbital and orbital cellulitis, meningitis, and sepsis.
Laryngomalacia/Tracheomalacia. Laryngomalacia refers to the collapse of supraglottic structures (arytenoid cartilage, epiglottis, etc.) during inspiration. It is the most common cause of congenital stridor with a diversity of anatomic etiologies. The stridor usually is loudest around the first or second months of life and resolves by the first or second birthday. The stridor is increased with agitation or supine positioning and decreases when the infant is in the prone position. The presence of an acute respiratory infection or gastroesophageal reflux may increase the stridor. These infants may have retractions, tachypnea, poor feeding, and failure to thrive. If the latter are present, the infant should be referred to an otolarygologist (ENT) for further evaluation and management. Tracheomalacia is due to weakness of airway cartilage with dynamic collapse of the trachea during respirations. Because most tracheomalacia lesions are intrathoracic, they cause expiratory wheezing. The management is supportive. Supine positioning is recommended if respiratory distress is present. Bronchodilatory medications, such as albuterol, may worsen the wheezing and respiratory distress associated with tracheomalacia by relaxing the airway smooth muscles and, therefore, should be used cautiously in these children.
CME Question
An infant presents with noisy breathing and shortness of breath. On examination, the infant has inspiratory stridor with suprasternal and subcostal retractions. The parent states that he usually has noisy breathing but it has worsened since he developed runny nose and nasal congestion. Which of the following statements regarding laryngomalacia is true?
- Laryngomalacia is the collapse of supraglottic structures during inspiration, causing inspiratory stridor.
- The stridor improves in the prone position.
- Severe cases may have tachypnea, retractions, poor feeding and failure to thrive.
- The stridor is often exacerbated by an acute respiratory infection.
- All of the above.
