Congenital Anomalies: Neurologic Emergencies
Core Content: Emergency Management of Congenital Anomalies
- Know the anatomy and pathophysiology relevant to emergency management of congenital anomalies
- Know the indications and contraindications for emergency management of congenital anomalies
- Plan the key steps and know the potential pitfalls in the emergency management of congenital anomalies
- Recognize the complications associated with the emergency management of congenital anomalies
Neurologic Emergencies
Seizures. Seizures in the neonatal period are often associated with significant illness or brain pathology. They occur in up to 1-2% of term newborns and 10- 20% of premature infants. The newborn brain is immature at birth and is still in the process of cortical organization. The brain stem and diencephalon are more developed than the cortical structures causing distinct types of seizures. Seizures in the neonate may have a subtle presentation including lip smacking, chewing, eye deviation, autonomic dysfunction, and stereotypical movements such as stepping, pedaling, or swimming. The most common seizure type in the neonate is a clonic seizure, which is a slow, rhythmic, jerky movement of the facial, extremity, and axial muscles. Tonic seizures are less common and involve a single extremity or less commonly all extremities. Myoclonic seizures present with rapid twitches or jerks of the flexor muscle groups usually. Myoclonic jerks occurring during sleep or upon waking are regarded as benign.1
|
Hypoxic ischemic injury: perinatal asphyxia, focal infarction, or stroke |
|
Infections: TORCH infections, CNS infections |
|
Electrolyte abnormalities: hyponatremia, hypoglycemia, hypocalcemia, hypomagnesemia |
|
Inborn errors of metabolism: amino acid disorders, organic acidurias, mitochondrial disorders, peroxisomal disorders, glucose transport (GLUT1) deficiency |
|
Intracranial hemorrhage: intraventricular, parenchymal, subdural, subarachnoid |
|
Congenital brain malformations: microcephaly, Sturge-Weber syndrome, tuberous sclerosis, neurofibromatosis |
|
Pyridoxine (vitamin B6)-dependent seizure, folinic acid responsiveness syndromes |
|
Neonatal abstinence syndrome: drug withdrawal from narcotics such as methadone, heroin, propoxyphene, or opiates |
|
Kernicterus |
|
Hypertension |
|
Epilepsy syndromes: benign idiopathic neonatal seizures, benign familial neonatal seizures, early myoclonic epilepsy, Ohtahara syndrome (early infantile epileptic encephalopathy), or Coppola-Dulac syndrome (malignant migrating partial seizures in infancy) |
CME Question
A 2-week-old infant presents to the emergency department with episodes of lip smacking and eye deviation. Regarding seizures in this age group, which of the following statements is true?
- Generalized tonic-clonic seizures are common.
- Myoclonic jerks during sleep or on waking are usually pathologic.
- The birth history is usually unremarkable.
- Lip smacking, chewing, eye deviation and stereotypical movements may occur.
Start or Resume CME Test (Opens in a new Tab/Window)
Management of Neonatal Seizures. A careful history may suggest the underlying etiology of the seizures and should include family history, prenatal and intrapartum events, maternal and infant infections, substance abuse, and presence of prenatal care. Dietary history is particularly important (breast milk vs formula; how formula is prepared). Use of home remedies and/or over-the-counter medications should be elicited.
The physical examination should include a full neurologic exam, including newborn reflexes such as the Moro reflex. The skin exam may reveal bruising caused by trauma, café au lait spots, cranial hemangioma, or herpetic lesions. The presence of an unusual odor of sweat or urine may indicate an inborn error of metabolism. A cranial bruit may be a sign of an arteriovenous malformation (AVM). Seizures in the newborn should prompt a thorough investigation into the etiology. This should include electrolyte levels, testing for certain inborn errors of metabolism, infectious disease work-up, toxicologic evaluation, neurological consultation, radiologic imaging of the brain (CT or MRI), and EEG monitoring. The infant should be admitted for further management. Perinatal events such as low Apgar scores, meconium-stained amniotic fluid, and prolonged labor pose an increased risk for perinatal asphyxia and hypoxic ischemic encephalopathy (HIE). These infants often develop seizures and developmental delay. CT of the head may reveal cerebral infarct or atrophy. An actively seizing or postictal patient requires immediate attention and careful monitoring of the airway, breathing, and circulation. Oxygen should be administered. A bedside glucose test will identify life-threatening hypoglycemia. Intravenous or intraosseous access should be established quickly2 and 0.5-1 g/kg of dextrose (5 mL/kg of D10%) should be administered for hypoglycemia. The choice of first-line anti-epileptic medications for the neonate on status epilepticus is controversial. Traditionally, phenobarbital (15-20 mg/kg) has been considered the first-line agent of choice.3 However, many providers prefer to use benzodiazepines (diazepam, lorazepam, or midazolam) first because of their rapid onset. Cardiorespiratory monitoring is mandatory in these infants since respiratory depression is common. Phenytoin or fosphenytoin is an alternative for resistant status epilepticus. Electrolyte and/or metabolic derangements (hypo-/hypernatremia, hypocalcemia, hypomagnesemia, pyridoxine deficiency) should be acutely corrected.
National Guidelines/Academic Resource
http://apps.who.int/iris/bitstream/10665/77756/1/9789241548304_eng.pdf
CME Question
A 1-month-old infant presents to the emergency department by EMS. The infant is actively seizing. Intravenous access is obtained. A bedside glucose is 75. Important steps in the management of this infant include all of the following except:
- Airway management and supplemental oxygen.
- Administration of dextrose 10% 5 mL/kg.
- Administration of phenobarbital 20 mg/kg.
- Administration of lorazepam 0.05-0.1 mg/kg.
Start or Resume CME Test (Opens in a new Tab/Window)
Intracranial infections or sepsis may cause seizures in the newborn. The most common bacterial infections in the neonatal period are E. coli and group B streptococcus. S. aureus and Listeria monocytogenes are less common. TORCH infections, especially toxoplasmosis and congenital rubella commonly cause seizures. Cytomegalovirus (CMV) and Coxsackie virus infections may cause seizures in the first week of life. Herpes simplex virus (HSV) usually occurs after the first week of life and should be considered in any neonate with seizures, vesicular rash, maternal history of HSV infection, or CSF leukoctyosis with a negative gram stain. If infection is suspected, CSF analysis for cell count and culture should be done. Broad-spectrum empiric antibiotics should be given pending culture results, usually ampicillin (50 mg/kg) plus cefotaxime (50 mg/kg) or gentamicin (2.5 mg/kg). Acyclovir (20 mg/kg) should be administered if HSV is considered until viral culture or polymerase chain reaction (PCR) results are available.
National Guidelines/Academic Resources
http://pediatrics.aappublications.org/content/129/5/1006.full
CME Question
A 4-day-old infant presents to the ED with fever and irritability and a focal seizure. On examination of the infant, a vesicular rash is noted on the face and scalp. Which statement is true regarding this infant?
- A full sepsis workup is recommended with administration of ampicillin and cefotaxime.
- CSF leukocytosis with a negative gram stain may occur.
- Acyclovir 20 mg/kg/dose intravenously.
- CSF cultures or PCR for herpes virus should be performed.
- All of the above.
Start or Resume CME Test (Opens in a new Tab/Window)
Hyponatremia in the newborn may result from improper preparation of formula (over-dilution) or inappropriate administration of free water to an infant. A careful feeding history and method of formula preparation should be obtained. Syndrome of inappropriate ADH secretion (SIADH), cystic fibrosis, malabsorption, or diarrhea may also cause sodium derangements resulting in seizures. Seizures caused by hyponatremia do not respond to benzodiazepines or anti-epileptic medications. A basic metabolic panel will confirm the abnormal sodium level. In the actively seizing neonate, treatment is 3% sodium chloride (3-5 mL/kg) with the goal to increase the sodium level just above the seizure threshold. Rapid correction of sodium level should be avoided since it may result in central pontine myelinosis.
CME Question
A 5-day-old infant presents to the ED with a history of decreased activity and lethargy. While in the ED, the infant has a seizure. The chemistry panel reveals a sodium level of 120. Concerning the treatment of this infant, which of the following statements is false?
- Administration of lorazepam 0.05 mg/kg will control the seizure.
- Administration of 3% sodium chloride 5 ml/kg is recommended.
- The feeding history is important, especially regarding formula preparation.
- Examination for ambiguous genitalia is important.
Start or Resume CME Test (Opens in a new Tab/Window)
Hypocalcemia may occur in the first few days of life in infants of diabetic mothers, intrauterine growth retardation, perinatal asphyxia, or prematurity and may cause focal seizures and irritability.4 Late onset, usually after 10 days, may occur in congenital hypoparathyroidism, DiGeorge syndrome, mitochondrial disorders, and hypomagnesemia. Hypocalcemic seizures are treated with calcium gluconate 10% (100-200 mg/kg or 1-2 mL/kg IV) slowly over 5-10 minutes, with cardiorespiratory monitoring. Alternatively, calcium chloride 10% (20 mg/kg or 0.2 mL/kg IV) may be administered.
Hypomagnesemia may cause refractory hypocalcemia. In order to successfully correct the hypocalcemia in these patients, the low magnesium levels must be addressed first Magnesium sulfate 12.5% is given (50-100 mg/kg) intravenously.
CME Question
An infant with Tetralogy of Fallot and abnormal facies presents to the ED with irritability. The evaluation of this infant reveals a low serum calcium. Which statement is true regarding this patient?
- DiGeorge syndrome must be considered.
- Treatment is with calcium gluconate 30% (1-2 mL/kg) slowly over 5 to 10 minutes, with cardio-respiratory monitoring.
- Magnesium levels are irrelevant in treating low calcium levels.
- Hypercalcemia is common
Start or Resume CME Test (Opens in a new Tab/Window)
Hypoglycemia in the newborn is generally defined as a blood glucose of < 45 mg/dL in the first 24 hours of life and < 50 mg/dL after 24 hours. Hypoglycemia may result from high circulating levels of insulin or high utilization of glucose. It is a common complication in infants of a diabetic mothers and is usually noted shortly after birth. Early feeding is recommended in these infants. Infants who are large or small for gestational age are also at risk for hypoglycemia. Inborn errors of metabolism, endocrinopathies, and infections may also result in hypoglycemia. Treatment is 0.5-1 g/kg of dextrose (2.5-5 mL/kg of D10% solution). More concentrated dextrose solutions (D12.5%; D50%) may be caustic to the neonate’s peripheral veins and should be administered only via central lines.
National Guideline/Academic Resource
http://pediatrics.aappublications.org/content/127/3/575.full.pdf+html
CME Question
A 4-day-old infant is brought to the ED by EMS for poor feeding and lethargy. On arrival in the ED, the infant has an episode of lip smacking and apnea. The infant is intubated. A bedside glucose level is 45. The best appropriate treatment is:
- Dextrose D50% intravenously 1 mL/kg.
- Dextrose D25% intravenously 2 mL/kg.
- Dextrose D10% 4 -5 mL/kg.
- Dextrose D5% 10 mL/kg.
Start or Resume CME Test (Opens in a new Tab/Window)
Inborn Errors of Metabolism (IEMs) are genetic defects resulting in the deficiency of certain metabolic enzymes and an excess or deficiency of a metabolite.5 There are more than 400 identified IEMs. All U.S. states provide mandatory newborn screening for some of the more common abnormalities, but there is no universal standard testing. Additionally, the screening test results are sometimes not available when the infant becomes symptomatic and presents to the health care system within the first week of life. Vomiting, lethargy, seizures, and shock are the most common presenting symptoms. The parents may note a strange odor to the newborn such as sweaty feet (isovaleric academia) or sweet smelling urine (maple syrup urine disease). Dysmorphic features may be evident on examination. These infants usually present with hypoglycemia, ketosis, and metabolic acidosis due to abnormalities in carbohydrate metabolism or fatty acid oxidation. Hyperammonemia is associated with urea cycle defects. Laboratory testing should include glucose, complete metabolic panel, ammonia, lactate, serum amino acid, urine amino acids, urine ketones, as well as CSF lactate, pyruvate, and glycine levels. Emergency treatment includes reversing cardiovascular shock, treating seizures, and correcting life-threatening metabolic and electrolyte derangements. Chronic management is tailored to the specific disorder but often involves diet modification.
CME Question
A 4-day-old infant with jitteriness and blood glucose of 45 is noted. The parents state that the infant has a strange sweet smell. The birth history was unremarkable. The bedside blood sugar is 45. Which of the following statements for this group of disorders is true?
- Newborn screening is identical in all states in the U.S.
- Hypoglycemia is a common finding.
- The diagnosis is often known prior to first ED presentation.
- All of the above.
Start or Resume CME Test (Opens in a new Tab/Window)
National Guideline/Academic Resource
http://onlinelibrary.wiley.com/doi/10.1046/j.1440-1754.2002.00047.x/pdf
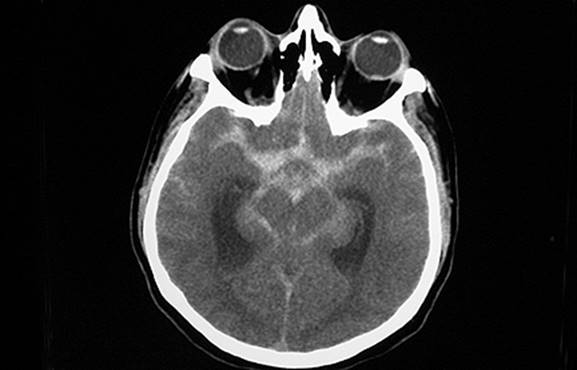
Intracranial hemorrhage in an infant may present with seizures, lethargy, vomiting, or a bulging fontanelle.6 (See Figure: Intracranial Hemorrhage) It occurs more frequently in the premature infants (intraventricular hemorrhage). Infants who have not received appropriate vitamin K therapy at birth are also at increased risk for intracranial hemorrhage. In the term infant, intracranial hemorrhage may occur due to accidental or non-accidental trauma. A skeletal survey and ophthalmology consult to rule out retinal hemorrhages should be done if non-accidental trauma is suspected.
CME Question
A 3-week-old is referred to the ED by the pediatrician for scalp swelling. The mother states that while in the care of her boyfriend, the infant rolled off the bed unto the tile floor. Which statement is true regarding this infant?
- The presence of a bulging fontanel, lethargy and vomiting are suggestive of increased intracranial pressure.
- The injury is suspicious for non-accidental trauma.
- A CT brain is recommended.
- All of the above
Start or Resume CME Test (Opens in a new Tab/Window)
Pyridoxine deficiency, an autosomal recessive condition, is rare but, when present, causes seizures in the neonates Pyridoxine deficiency results in decreased GABA (an inhibitory neurotransmitter) synthesis. A pregnancy history may reveal episodic staccato movements during the pregnancy. The infant usually presents with seizures hours after delivery. The infants are often agitated and may have vomiting, respiratory distress, and metabolic acidosis. A trial of intravenous pyridoxine is recommended for unexplained refractory seizures not responding to conventional anti-seizure medications. Close monitoring is required and these infants may require oral pyridoxine for several weeks.
CME Question
An infant had refractory seizures in the newborn period, responding to intravenous pyridoxine. Which statement is true regarding this infant?
- Oral pyridoxine may be required for several weeks.
- Phenobarbital is often appropriate treatment of the seizures.
- The disorder is thought to be an autosomal dominant condition.
- The seizures usually occur several days after birth.
E.All of the above.
Start or Resume CME Test (Opens in a new Tab/Window)
Neonatal Abstinence Syndrome: Maternal drug use during pregnancy, legal or illegal, can have deleterious effects on the fetus. The most common illegal drugs abused in the United States are cannabinoids, cocaine, heroin, and methamphetamines. Recently, there has been an increase in narcotic abuse and methadone treatment in the United States, with significant impact on the neonatal population.7 Maternal drug use is more commonly associated with poor or absent prenatal care, precipitous delivery, placental rupture, and preterm labor. Consequences for infants born to mothers who abused drugs during pregnancy include congenital malformations, intrauterine growth retardation, acute withdrawal syndromes, neurobehavioral effects, and neonatal stroke, among others. The effects of acute drug withdrawal may occur shortly after birth, within 24-48 hours, and as late as two weeks after delivery.8 The latter are more likely to present in the ED with various neurologic, cardiovascular, and gastrointestinal complaints such as irritability, jitteriness, high pitched cry, tremors, seizures, increased or decreased tone, increased or decreased reflexes, increased or decreased suck, lethargy, fever, sweating, tachycardia, tachypnea, cyanosis, nasal congestion, vomiting, diarrhea, weight loss, or increased appetite. The severity depends on the number of drugs abused and the timing of last dose prior to delivery. The diagnosis may be supported by a positive urine toxicology screen in the infant, but has limited value after several days. Meconium and hair analysis may be obtained for confirmation of drug exposure, but are expensive and the results are not immediately available. Diagnosis is supported mostly by a thorough history as well as exclusion of other etiologies. Symptomatic treatment, including swaddling, rocking, and increased caloric intake, is effective in some cases. More severe cases are treated with medications, including lorazepam, phenobarbital, morphine, and methadone. Standardized scoring systems are used to track an infant’s withdrawal symptoms and clinical progress. Social services should be involved in all cases in which a pregnant woman has been abusing drugs.
National Guideline/Academic Resource
http://pediatrics.aappublications.org/content/133/5/937.2.full?rss=1
CME Question
A 2-week-old female infant is in foster care because of child neglect reported for the other siblings. She presents with irritability, tremors, and frequent spitting up of feeds. The mother had no prenatal care and a history of drug use. The infant was born at another facility. Urine drug screen on the mother was negative but done after 72 hours when consent was obtained. A true statement regarding this infant is:
- Neonatal abstinence syndrome usually occurs at 12 weeks of age.
- Infants are usually large for gestational age.
- Symptoms include seizures and vomiting.
- The maternal urine drug screen is always positive.
Start or Resume CME Test (Opens in a new Tab/Window)
Botulism. Infants may be colonized with Clostridium botulinum spores after ingestion. The disease peaks at about 2-4 months of age but may present as early as 3 days. Risk factors include ingestion of honey and parents who work in agriculture and live in rural areas. Botulinum toxin binds to and irreversibly blocks cholinergic receptors. Symptoms of botulism include constipation, hypotonia, cranial nerve abnormalities, flaccid paralysis (descending), and autonomic instability. A stool assay is used for the diagnosis. Treatment is supportive: ventilation and nutritional support. Use of drugs that prolong cholinergic blockade (e.g., gentamicin) should be avoided. BabyBIG, human-derived botulinum immune globulin, is available for use in children less than 1 year of age (equine serum botulism antitoxin is available for older children) and should be administered as soon as possible, as it significantly decreases the length of the hospital stay by about 50%.
CME Question
A 1-month-old infant is referred to the ED from a rural farming community. The infant has constipation, poor tone, and a weak cry. You suspect botulism. Which is true about this condition?
- Symptoms are due to the blockade of cholinergic receptors.
- Treatment is mainly supportive.
- Baby botulinum immune globulin (baby BIG) decreases hospital stay by 50%.
- Diagnosis is by stool assay.
- All of the above.
Start or Resume CME Test (Opens in a new Tab/Window)
| Drug | Dose | Maintenance |
|---|---|---|
| Lorazepam |
0.05 to 0.1 mg/kg/dose (max 2 mg) IV over 2-5 min May repeat in 10-15 min x 1 dose |
|
| Diazepam |
0.3 to 0.75 mg/kg/dose (max 2 mg) IV May repeat in 15-30 min x 2-3 doses |
0.3 mg/kg/hour continuous infusion |
| Midazolam | 0.1 to 1.1 mg/kg/hour | 0.1 to 1.4 mg/kg/hour continuous infusion |
| Phenobarbital |
20 mg/kg/dose IV May give additional 5 mg/kg doses in 15- to 30-min intervals Max total dose 40 mg/kg. |
3 to 4 mg/kg day IV daily or divided BID Check levels |
| Phenytoin or fosphenytoin |
20 mg/kg/dose IV
Administer phenytoin slowly |
3 to 4 mg/kg/day IV divided BID to 4 times daily Check levels |
| Levetiracetam (Keppra) | 20 mg/kg/dose IV | 10 mg/kg/day IV divided BID and titrate up to 40 mg/kg/day |
| Etiology | Risk Factors | Diagnosis | Treatment |
|---|---|---|---|
| Hypoglycemia |
Infant of diabetic mother, small or large for gestational age, intrauterine growth retardation, inborn errors of metabolism |
Glucose check < 45-50 mg/dL |
Dextrose 10% (2 to 4 mL/kg) IV |
| Hyponatremia | Formula-fed infant, congenital adrenal hyperplasia, syndrome of inappropriate antidiuretic hormone due to hypoxic ischemic encephalopathy |
Chemistry panel: Na (usually < 125) |
Sodium chloride 3% IV 3 to 5 mL/kg |
| Hypocalcemia |
Infant of diabetic mother, intrauterine growth restriction, perinatal asphyxia, prematurity, hypomagnesemia, hypoparathyroidism, high-phosphate formula, DiGeorge syndrome |
Calcium level |
Calcium gluconate 10% IV 1 to 2 mL/kg over 5-10 minutes May repeat x 1 Cardiac monitor |
| Hypomagnesemia | Hypocalcemia | Magnesium levels |
Magnesium sulfate 12.5% IV 50 to 100 mg/kg over 1-2 hours to correct level < 1 to 6 mg/dL Cardiac monitor. |
|
Inborn errors of metabolism Pyridoxine (B6)-responsive seizures Pyridoxal phosphate-responsive seizures |
Dysmorphic features, strange odor, family history of inborn errors of metabolism. | Complete metabolic panel: decreased glucose, acidosis, increased ammonia level, increased lactate level, serum amino acids, urine amino acids, urine ketones, CSF lactate, pyruvate, glycine. |
Non-ketotic hyperglycinemia is treated with sodium benzoate 250 to 750 mg/kg/day to decrease levels of glycine in combination with dextromethorphan 5 to 20 mg/kg/day Or memantine to block glycine effects on NMDA receptors |
|
Pyridoxine (B6)-responsive seizures Pyridoxal phosphate-responsive seizures. Folinic acid-responsive seizures |
Family history of inborn errors of metabolism, unexplained neonatal death in sibling, parental consanguinity | Complete metabolic panel: decreased glucose, acidosis, increased ammonia level, increased lactate level, serum amino acids, urine amino acids, urine ketones, CSF lactate, pyruvate, glycine. |
Pyridoxine responsive seizures (i.e., deficiency of alpha AASA, PNPO deficiency) treated with pyridoxine 100 mg IV or 30 mg/kg PO May substitute pyridoxal phosphate 10 mg/kg IV or 30 mg/kg/day PO Some patients who don’t respond to pyridoxine may respond to pyridoxal phosphate Folinic acid-responsive seizures treat with folinic acid 2.5 mg/kg/day IV |
| Neonatal Abstinence Syndrome (NAS) |
Maternal drug use, poor prenatal care |
Urine toxicology, meconium or hair assay. Symptoms in neonate such as jitteriness and seizures. |
Swaddling, quiet low light environment, rocking For active seizures lorazepam 0.05 to 0.1 mg/kg/dose IV over 2-5 mins. Repeat if necessary Phenobarbital 20 mg/kg/dose IV Morphine, opium, paregoric are options utilized in different centers Avoid naloxone in infant with maternal methadone use. May precipitate seizure. |
National Guidelines/Academic Resources
http://apps.who.int/iris/bitstream/10665/77756/1/9789241548304_eng.pdf
Neurologic Emergencies References
- Silverstein ES, Jensen FE. Neonatal seizures. Ann Neurol 2007: 62:112-120.
- Newborn Nursery QI Committee. Portland (ME):The Barbara Bush Children’s Hospital at Maine Medical Center: 2004 Jul. Neonatal hypoglycemia: initial and follow up management. National Guideline Clearing house 2004.
- Painter MJ, Scher MS, Stein AD, et al. Phenobarbitol compared with Phenytoin for the treatment of neonatal seizures. N Engl J Med 1999, 341:485-489.
- Gertner JM.Disorders of calcium and phosphorus homeostasis. Pediatr Clin North Am 1990: 37:1441-1465.
- Ellaway CJ, Walden B,Chistodoulo J. Inborn errors of metabolism: Neonatology for the generalist: Clinical approach of inborn errors of metabolism presenting in the newborn period. J Pediatr Child Health 200238:511-517.
- Jayawant S, Rawlinson A, Gibbon F, et al. Subdural hemorrhages in infants. Population based study. BMJ 1998:317:1558-1561.
- Patrick SW, Schumacher RE, Benney-worth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures. United States, 2000-2009. JAMA 2012:301(18):1934-1940.
- Kendall SR, Gartner LM.Late presentation of drug withdrawal syndromes in newborns. Am J Dis Child 1974:127(1):58-61.
