Neurologic Trauma
Module 3: Pediatric Trauma
Authors
Whitney Kiebel, MD, Resident, Departments of Pediatrics and Emergency Medicine, University of Arizona, Tucson, AZ
Aaron Leetch, MD, Assistant Professor, Departments of Emergency Medicine and Pediatrics; Associate Program Director, Emergency Medicine/Pediatrics Residency, University of Arizona, Tucson, AZ
Dr. Kiebel and Dr. Leetch report no financial relationships relevant to this field of study.
Core Content Outline: Central Nervous System — Blunt Head Trauma
Etiology
-
Know common etiologies of blunt head trauma in children, excluding non-accidental trauma
Pathophysiology
-
Understand the mechanisms leading to increased intracranial pressure following blunt head trauma
-
Understand the significance and complications of skull fracture
Recognition
-
Plan the evaluation and management of basilar skull fractures
-
Recognize the signs and symptoms of intracranial hemorrhage following blunt trauma
-
Recognize the signs and symptoms of increased intracranial pressure and cerebral herniation following blunt head trauma
-
Recognize respiratory insufficiency in patients with head trauma
-
Recognize and interpret computed tomography of the head in a patient with blunt head trauma
-
Know the indications for magnetic resonance imaging of the head in blunt head trauma
-
Know the indications for computed tomography of the head in a patient with blunt head trauma
Management
-
Plan treatment priorities in the management of children with head injuries due to blunt trauma
-
Know the role of pharmacology in the management of children with head injuries due to blunt trauma
-
Know the role of surgery in the management of children with head injuries due to blunt trauma
-
Plan airway management for children with head injuries due to blunt trauma
-
Know the management of increased intracranial pressure following blunt trauma
-
Know the principles of management using hyperventilation after severe blunt head injury
-
Know the principles of the management of cerebral contusion
-
Know the principles of the management of minor head injury
Central Nervous System – Penetrating Head Trauma
Etiology
-
Know the most common life-threatening causes of penetrating head injuries in children
Pathophysiology
-
Understand the relationship between ballistics and penetrating injury to the brain
Recognition
-
Recognize the signs of increased intracranial pressure in a child with a penetrating injury to the central nervous system
-
Recognize the potential for infection following penetrating injury to the central nervous system
Management
-
Know the indications for radiographic studies in evaluating the condition of children with penetrating injuries to the head
-
Plan the management of children with penetrating injuries to the head
Pediatric Head Trauma
Etiology
Head injury is a major cause of morbidity and mortality in children. The Centers for Disease Control and Prevention estimates there are more than 7000 pediatric deaths annually. In addition, nearly 40% of all trauma-related deaths in children are secondary to traumatic brain injury (TBI).
Studies have shown that the incidence of TBI in children has a bimodal distribution, peaking in children ≤ 4 years and between 10-17 years of age.
Falls are the most common etiology of head injuries seen in toddlers, whereas motor vehicle accidents are most commonly the cause of TBI in adolescents.
Non-accidental trauma is a common cause of TBI in infants younger than 1 year of age.
The highest rates of morbidity and mortality occur in children < 4 years of age and in those who present with a low Glasgow Coma Scale (GCS) score, coagulopathy, hypotension, or hyperglycemia. Mortality among children has been reported to be lower than that in adults. However, disability and long-term functional outcome may be significantly impacted.
CME Question
6. A 7-month-old male presents to the emergency department with his 18-year-old mother for fussiness for 2 days. Today, the patient is lethargic, and his mother is having a difficult time waking the baby. The patient exhibits hypertonicity and is minimally responsive. He does not have any external signs of trauma. Pupils are sluggish and dilated. He has shallow respirations. He had been meeting his milestones and feeding well prior to this episode. Of the following which scenario is most likely?
-
The child suffered a head injury from a fall.
-
The child is a victim of a non-accidental trauma.
-
The child has retinal hemorrhages.
-
The child has an epidural hematoma.
-
Both a and d
-
Both b and c
Start or Resume CME Test
(Opens in a new Tab/Window)
Pathophysiology
Pediatric patients exhibit an exaggerated cerebrovascular response to TBI compared to adults. The pathophysiology of TBI may be divided into two phases: primary and secondary injury.
The primary event is the direct injury to the brain parenchyma. The secondary injury involves the cascade of events that occur as a result of the initial insult, including biochemical, metabolic, and cellular responses. Secondary injury may be exacerbated by hypoxia, hypotension, and other systemic derangements.
Increased intracranial pressure and herniation
Cerebral edema and intracranial hemorrhage (ICH) are common causes of increased intracranial pressure (ICP). Symptoms of increased ICP occur after compensatory mechanisms (i.e., blood pressure autoregulation) have been exhausted. Symptoms may manifest as headache, nausea, vomiting, altered mental status, and/or posturing.
Secondary/reactive injury occurs as a result of vascular autoregulation dysfunction, cerebral edema, increased intracranial pressure, expanding hemorrhage, or ischemia from seizures. Diffuse edema/swelling of the brain tissue is more common in children compared to adults, as release of excitatory neurotransmitters, which may be exaggerated in the developing brain, worsens the neuronal injury.
The primary cause of secondary brain injury is increased ICP and decreased cerebral perfusion pressure (CPP), which is a function of mean arterial pressure (MAP) and ICP.
CPP = MAP - ICP
The Monroe-Kellie Doctrine states that the total volume of the brain is static, consisting of intravascular blood, brain parenchyma, and cerebrospinal fluid. (CSF). If additional volume is introduced (extravascular blood or mass lesion) or the volume of an existing structure is increased (cerebral edema or increased CSF volume secondary to obstructed outflow), the surrounding volumes must decrease in order to maintain constant ICP. When this compensation fails, ICP increases. This will initially lead to a decrease in cerebral blood flow and brain ischemia. As pressure continues to rise, brain herniation occurs.
Cerebral herniation may occur through the tentorial incisura, the inferior edge of falx cerebri or the foramen magnum. Central transtentorial herniation is the most common location of herniation.
The progression of the herniation process is as follows:
Diencephalon and upper brainstem compressed → deterioration in LOC, respiratory irregularity, pupillary dilation, upward gaze limitation and hypertonia → continued caudal progression → decorticate posturing, pupillary dilation and hyperventilation develop → then basilar artery compression and brainstem ischemia
Normal intracranial pressure is < 20 mmHg.
When managing head injuries, the goal is to maintain an ICP <15 mmHg if possible, although some literature supports < 20 mmHg.
The goal is to keep the CPP > 40 mmHg. Because the autoregulatory mechanisms are altered after TBI, maintaining an adequate blood pressure is essential to maintaining the cerebral perfusion.
National Guideline/Academic Resource
The injured pediatric brain has increased metabolic demand compared to adults, which places it in a vulnerable state. Secondary insults such as hypotension, hypoxemia, seizures, hyperthermia, and hypoglycemia can devastate the injured brain. Although hyperventilation can temporarily decrease ICP, hyperventilation to a PaCO2 level < 35 mmHg offers little benefit and < 25 mmHg can be harmful. This is thought to be secondary to a reduced cerebral blood flow.
Approximately 10% of children experience post-traumatic seizures after TBI. Though immediate and early seizures do not have any prognostic significance, they may require anticonvulsant therapy to prevent further insult and to decrease the metabolic demand. Late post-traumatic seizures likely occur from cortical scarring and are a negative prognostic indicator.
CME Question
7. An 18-year-old presents after suffering a traumatic brain injury. She has an ICP monitor in and is persistently > 30 mmHg. She has also been intermittently hypotensive. Which of the following statements is true?
-
In this age group, motor vehicle accidents are the most common cause of TBI.
-
She should receive hypertonic saline.
-
She should be hyperventilated before receiving hypertonic saline.
-
She should receive steroids.
-
Both a and b
-
Both b and d
-
All of the above
Start or Resume CME Test
(Opens in a new Tab/Window)
Types of Head Injury
Skull Fractures
Skull fractures often accompany pediatric head trauma. These can be either open or closed. An open fracture involves an overlying laceration whereas a closed does not. Open fractures are treated with surgical debridement if they are depressed and underlying dura or brain is lacerated.
|
Skull fracture: TYPE |
|
|
|
|
Etiology |
|
|
|
|
Signs/ Symptoms |
|
|
|
|
Treatment |
|
|
|
CME Question
8. A 5-year-old boy is brought to the emergency department after suffering a fall from a bunk bed. He has been complaining of a mild-moderate headache since the fall. His neurologic exam is unremarkable, including cranial nerves. He has hemotympanum on the right and raccoon eyes. You are concerned for a basilar skull fracture. Besides confirming this with a CT scan, what else should you do?
-
Call neurosurgery immediately for an emergent consult and operative intervention
-
Elevate the head of the bed
-
Place a nasogastric tube to decompress his stomach, as he is at risk for aspiration
-
Begin antibiotics immediately
-
All of the above
Start or Resume CME Test
(Opens in a new Tab/Window)
Concussion
A concussion is defined as a transient state of neuronal dysfunction from traumatic injury. It involves a complex constellation of symptoms, ranging from transient confusion to loss of consciousness with deep stupor. Concussive syndrome may involve skin pallor, increased sleepiness, nausea, vomiting, ataxia, mood swings, dizziness, and difficulty concentrating. Symptoms typically will last 3-4 days, although younger children may have prolonged symptoms (7-10 days). It is common to have retrograde or anterograde amnesia.
|
Diagnostic Criteria for Mild Traumatic Brain Injury |
|
A patient with mild traumatic brain injury has had a traumatically induced physiologic disruption of brain function, as manifested by 1 or more of:
|
|
Adapted from the Mild Traumatic Brain Injury Committee of the American Congress of Rehabilitation Medicine |
|
Diagnostic Criteria for Post-Concussive Disorder |
|
|
No single test score can be the basis of a concussion diagnosis. Moderate evidence that standardized symptom checklists (Post-Concussion Symptom Scale/Graded Symptom Checklist [GSC]) and the Standardized Assessment of ©2013 American Academy of Neurology www.aan.com Concussion (SAC) when administered early after a suspected concussion have moderate to high sensitivity and specificity in identifying sports concussions relative to those of the reference standard of a clinician-diagnosed concussion. Low-moderate evidence that the Balance Error Scoring System (BESS) has low to moderate sensitivity and moderate to high specificity in identifying sports concussions. Those affected may have exacerbation of symptoms with mental or physical exertion. Adapted from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition. |
National Guideline/Academic Resource
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3303645/
Diffuse Axonal Injury
Diffuse axonal injury (DAI) is a more severe form of diffuse brain injury that results from tissue (myelin and axons) shearing at the grey and white matter interface and can cause significant neuronal injury. In children < 1 year of age, DAI is most commonly associated with shaken baby syndrome. This occurs from tearing of the anterior bridging veins and petechial hemorrhages in white matter and deep grey structures with shearing of myelin and axons. Contusions of the corpus callosum, subarachnoid hemorrhages, and intracranial hypertension may occur. Many of the infants who are victims of shaken baby syndrome will not present with any external signs of trauma. They can present with deep coma, decorticate posturing, dilated pupils, apnea, or bradycardia without computed tomography (CT) findings. Retinal hemorrhages are common and often diagnostic. In older children, DAI is usually a primary impact injury. Due to the significant shearing forces, there may be small intracranial hemorrhages (contusions and lacerations). Diffuse brain edema and the disruption of the blood brain barrier occur.
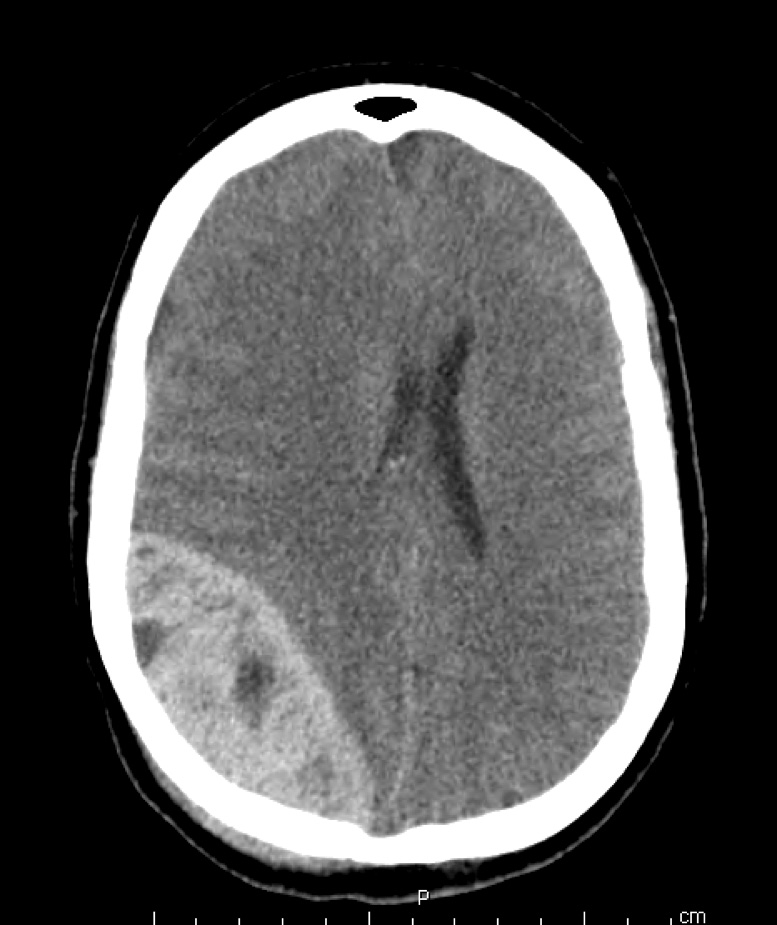
Epidural Hematoma
Epidural hematomas are rare (< 3% of pediatric head injuries) and most commonly result from a high fall onto a hard surface or a motor vehicle accident. In children < 5 years of age, epidural hematomas rarely present with the classic lucid period. Children may have a subacute presentation and begin to exhibit signs of increased ICP 48 hours after the injury. These hemorrhages most commonly result from a meningeal and diploic vein injury. Less commonly, they are associated with middle meningeal artery hemorrhage (unlike adults). Occasionally and typically after occipital trauma, an epidural hematoma may result from deep venous sinus hemorrhage in the posterior fossa. Patients present with nuchal rigidity, cerebellar signs, vomiting, and altered level of consciousness. Epidural hematomas are true neurosurgical emergencies. Only a select few small venous epidural hematomas can be managed conservatively. Nearly half of these hemorrhages involve skull fractures.
Figure 1 – Epidural Hematoma
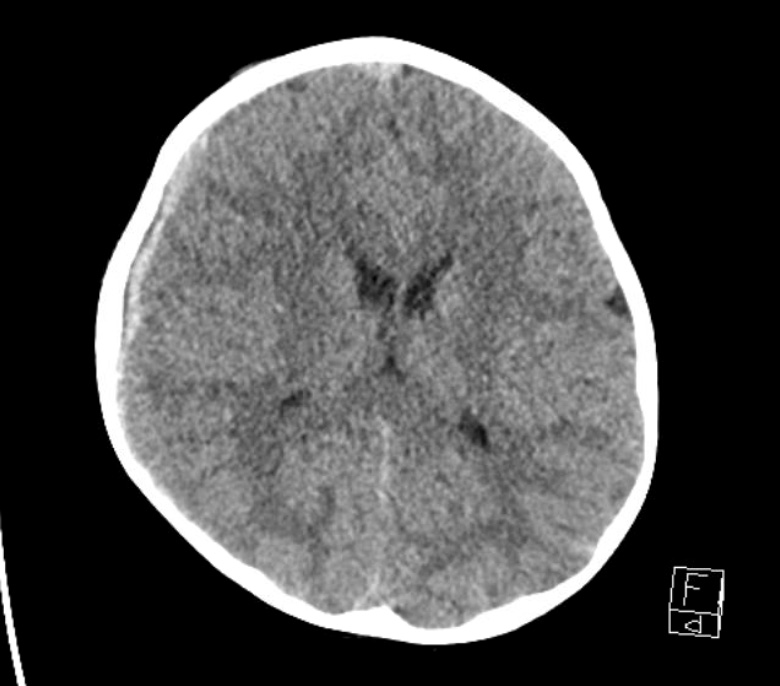
Subdural Hematoma
Subdural hematomas occur 5-10 times more frequently than epidural hematomas in children and are more common in infants. Most involve the cerebral bridging veins. In younger children, the presentation is usually subacute due to the plasticity of the pediatric skull. The subdural blood organizes into a hemorrhagic cyst over weeks and expands in size due to the osmotic pressure of the products of RBC breakdown. Children may develop macrocephaly without definite history of trauma and may present with seizures, lethargy, irritability, bulging fontanel, and retinal and pre-retinal hemorrhages. Older children present more acutely with symptoms of increased ICP.
Figure 2 – Subdural Hematoma
Cerebral Contusions
Cerebral contusions frequently follow acceleration/deceleration injuries and are found in the location of impact (coup) and/or on the opposite side of the brain (countercoup). As a result, cerebral contusions occur at the rostral frontal and temporal lobes and are commonly associated with cerebral edema. Temporal lobe contusions are potentially lethal due to their close proximity to the brainstem and can cause lateral herniation and death.
Brainstem Injuries
Brainstem injuries occur as a result of shear injuries, secondary to compression from adjacent traumatized brain tissue. The pressure differences between the supratentorial and infratentorial compartments place stresses on brainstem tissue. Central herniation can occur when the brainstem moves through the tentorial notch. Duret hemorrhages occur with tearing of vessels within the brainstem causing intraparenchymal hematomas and are usually lethal.
Recognition/Evaluation/Diagnosis
Assessment
Pediatric head trauma varies in severity from an uncomplicated minor TBI to a lethal traumatic brain injury. The ultimate goal is to prevent secondary injury, minimize morbidity and mortality, and improve neurologic outcome. The primary and secondary trauma surveys should be followed by a comprehensive neurologic exam.
-
General assessment
-
Pay attention to vital signs:
-
Respiratory rate and pulse oximetry: apnea/bradypnea or hypoxemia may reflect decreased level of consciousness, inability to protect airway, or insufficient respiratory drive
-
Bradycardia and hypertension may indicate impending herniation
-
Glasgow Coma Scale (GCS):
-
-
Table 1 – Glasgow Coma Scale (Infant GCS in italics)
|
Eyes |
Verbal |
Motor |
|
|
1 |
No response |
No response |
No response |
|
2 |
Open to pain |
Incomprehensible sounds Moans to pain |
Extension posturing (decerebrate) |
|
3 |
Open to speech |
Inappropriate words Cries to pain |
Flexion posturing (decorticate) |
|
4 |
Spontaneously open |
Confused Irritable |
Withdraws to pain |
|
5 |
- |
Oriented Coos, babbles, smiles, interacts |
Localizes to pain Withdraws to touch |
|
6 |
- |
Spontaneous movement |
-
The initial severity of TBI is determined by initial GCS score
-
Mild: GCS 13-15
-
Moderate: GCS 9-12
-
Severe: GCS < 8
-
-
Cranial nerve exam
-
Particularly pupils and CN III, as this may be a late sign of uncal hernation, if palsy present
-
Brainstem reflexes – if absent, may be indicative of severe life-threatening TBI
-
-
Pupillary response
-
CN II-III, VI-VIII, IX and X
-
Doll’s eye
-
Corneal reflexes
-
Gag reflex
-
Test motor reflexes, tone, and strength
-
Upper motor neuron injury: hyperactive reflexes and increased tone (spine injury)
-
Lower motor neuron injury: hypoactive reflexes and decreased tone (peripheral injury)
-
-
Diagnostic Evaluation
Laboratory evaluation depends on the injury mechanism and primary/secondary surveys. Most children with severe traumatic injuries require a CBC, hematocrit, type and screen, urinalysis, and coagulation studies. Arterial blood gas (ABG) may be useful in directing resuscitation. Hyperglycemia has been associated with poor outcomes, so this may be a useful prognostic test.
The decision to obtain imaging may be straightforward, if the mechanism and presentation are consistent with a severe brain injury. However, the clinical picture often is less clear. In such cases, the risks associated with imaging (i.e., CT-associated ionizing radiation) should be weighed against the benefits of the additional diagnostic data.
Some sources recommend advanced imaging for children with penetrating injury, persistent GCS of < 15, focal neurologic deficit, post-traumatic seizure, persistent vomiting, extensive facial injuries, or signs of basilar skull fracture. Other relative indications include loss of consciousness, abnormal sensorium, alcohol or drug intoxication, suspected child abuse, unreliable history, age < 2 years with significant mechanism, or skull fracture.
Validated rules can help with the decision to perform advanced imaging for intracranial injury in children. The largest study by the PECARN group included 42,412 children from 25 different emergency departments in the United States. The study included those presenting within 24 hours of injury with a GCS of 14-15. The goal was to identify children at low risk of clinically-important TBI who may not need a CT.
|
Table. Decision Rules for Avoiding CT in Children with Head Trauma |
|
|
< 2 years |
> 2 years |
|
Normal mental status |
Normal mental status |
|
No scalp hematoma except frontal |
No LOC |
|
LOC < 5 seconds |
No vomiting |
|
Non-severe injury mechanism* |
Non-severe injury mechanism* |
|
No palpable skull # |
No signs of basilar skull # |
|
Normal behavior |
No severe headache |
|
*Severe mechanism defined as MVA with patient ejection, death of a passenger, rollover; pedestrian or cyclist without helmet struck by motorized vehicle; fall > 1.5 m for children (> 2 years), fall > 0.9 m for < 2 years; or head struck by high impact object |
|
If none of the 6 predictors were present, the risk of ciTBI was <0.02%.
|
Canadian Assessment of Tomography for Childhood Head Injury: The CATCH Rule |
|
CT of the head is required for children with a minor head injury* plus any one of the following findings: |
|
High risk (need for neurological intervention)
|
|
Medium risk (brain injury on CT scan)
|
|
*Minor head injury is defined as an injury sustained within the past 24 hours associated with witnessed loss of consciousness, definite amnesia, witnessed disorientation, persistent vomiting (more than one episode), or persistent irritability (in a child younger than 2 years of age) in a patient with a Glasgow Coma Scale score of 13 to 15. CT = computed tomography |
Many injuries are easily diagnosed by CT. However, patients with diffuse axonal injury may have a normal CT but have an abnormal neurologic exam. In these cases, MRI may be a useful test following stabilization.
CME Question
10. An 18-month-old presents to the emergency department after suffering a fall. He fell off of the slide on the playground and hit his head on the cement. He was initially awake, but minimally responsive. Now he will only open his eyes and makes some moaning noises when someone pinches his hand and pulls his hand toward his chest when it is pinched. What is his Glasgow Coma Score?
-
9
-
8
-
7
-
10
Start or Resume CME Test
(Opens in a new Tab/Window)
Management
The primary goal of managing the severe TBI is identifying those injuries that will need urgent neurosurgical intervention and preventing secondary injury. After initial stabilization, severe TBI patients should be transferred immediately to a trauma center with expertise in caring for children. This includes those patients with a GCS ≤ 8, GCS ≤ 12, but with other serious injuries, or a decrease in GCS and deterioration in condition.
Airway/Breathing
Endotracheal intubation and mechanical ventilation may be required for stabilization and airway protection. In general, advanced airway management and ventilator support are recommended in patients with a GCS ≤ 8, respiratory distress or hypoxemia, or hemodynamic instability. Maintaining C-spine immobilization is imperative, as cervical spine injuries are more commonly associated with traumatic brain injuries. Use a cuffed endotracheal tube, as is now universally recommended.
Rapid Sequence Intubation (RSI) Consideration:
-
Pretreatment: Lidocaine if time permits (usually takes 2 minutes for full effect). Theoretically, this may decrease the risk of increased ICP associated with airway manipulation.
-
Sedative: Etomidate or ketamine (studies do not support a clinically significant increase in ICP associated with ketamine use) are preferred. Propofol and thiopental both have vasodilatory and negative inotropic effects and generally are not recommended.
-
Paralytic: Succinylcholine has been shown to increase ICP in patients with brain tumors, but this has not been shown in patients with traumatic brain injury. Rocuronium is also recommended but has a longer duration.
-
Ventilation: Hyperventilation (PaCO2 < 35 mmHg) can cause cerebral ischemia because of decreased cerebral blood flow. Thus, controlling the ventilation to maintain a PaCO2 between 35-38 mmHg is recommended unless there are signs of impending herniation.
National Guideline/Academic Resource
http://www.ncbi.nlm.nih.gov/pubmed/20473241
http://www.ncbi.nlm.nih.gov/pubmed/24515638
Circulation
It is important to manage hypovolemic and hemorrhagic shock to maintain cerebral perfusion. Several studies have shown that even a single episode of hypotension in children with severe TBI is associated with poorer outcomes. Replace volume with isotonic fluids. The target blood pressure has not been determined and is likely age dependent. The optimal CPP is unknown, but a minimum of 40-50 mmHg has been recommended. Age-specific endpoints should be considered (i.e., infants at the lower end; adolescents at the upper end of this range).
Other Methods to Improve Outcome
Other methods to improve outcome are targeted at maintaining CPP and preventing increased ICP. Elevating the head of the bed to 30 degrees (or reverse Trendelenburg if in spine precautions) and maintaining a neutral head position reduces neck vein compression and assists venous drainage from the brain. It is important to keep the child appropriately sedated and paralyzed to prevent increasing ICP secondary to agitation and anxiety.
Antiseizure prophylaxis is recommended with severe TBI to prevent early post-traumatic seizures.
Hyperthermia should be avoided and treated, as this increases metabolic demands.
Glucose should be maintained < 200.
Hyperosmolar therapy can be administered as a bolus or a constant infusion to decrease ICP. Options include hypertonic saline and mannitol. Because the blood-brain barrier is impermeable to sodium and mannitol, these work by osmotic effect, shifting fluid out of the confined cranial vault. Other potential benefits of these agents have been described.
The ideal acute bolus dose of hypertonic saline is unknown, but common initial doses of 3% saline are 3-10 mL/kg. Continuous infusions of 3% saline range between 0.1 and 1.0 mL/kg per hour. These are administered on a sliding scale, using the minimum dose needed to maintain ICP < 20 mmHg. Goal serum osmolality is < 360 mOsm/L. Adverse effects of hypertonic saline include hypertension, central pontine myelinolysis, and subarachnoid hemorrhage.
Mannitol remains a controversial drug. Some argue that it may accumulate in injured regions and draw fluid into the brain parenchyma, causing an increase in ICP. However, it has been demonstrated to be effective largely by small series in adults, and these data have been extrapolated to support their use in children. Doses range from 0.25-1 g/kg. Nephrotoxicity and hypovolemia can occur.
Hyperventilation can be used to reduce ICP, but indirect evidence has found that this may be harmful if practiced routinely in all patients with TBI. Hyperventilation causes hypocapnia, vasoconstriction, and resultant decreased cerebral blood flow. As a result, hyperventilation is only recommended for impending herniation.
Corticosteroids are not recommended and may increase mortality. There is a lack of benefit as well as potential harm for infectious complications and suppression of pituitary adrenal axis.
Hypothermia is not recommended routinely in TBI; however, moderate hypothermia (32-33 C) beginning within 8 hours after severe TBI for up to 48 hours duration should be considered to reduce intracranial hypertension. If hypothermia is induced, rewarming at a rate >0.5 C should be avoided.
Intracranial pressure monitoring is recommended for children with a GCS between 3-8, when interventions to decrease ICP are actively being performed, or when the practitioner is unable to perform serial neurologic exams because of pharmacologic sedation or anesthesia. This practice has been shown to improve outcomes in adults.
There is no evidence to support use of prophylactic barbiturates to prevent intracranial hypertension or for neuroprotective effects in children. High-dose therapy may be considered in hemodynamically stable, salvageable head injury patients with intracranial hypertension refractory to maximal medical and surgical ICP-lowering therapy.
National Guideline/Academic Resources
https://www.braintrauma.org/pdf/guidelines_pediatric2.pdf
https://www.braintrauma.org/pdf/protected/Guidelines_Management_2007w_bookmarks.pdf
http://www.guideline.gov/content.aspx?id=36899
Impending Herniation or Increased ICP
In the case of impending herniation or increased ICP, hyperosmolar therapy, ventilatory support, hemodynamic monitoring, mild hyperventilation (PaCO2 35-38 mmHg), and immediate neurosurgical evaluation are recommended.
Minor Head Trauma
Minor head traumas are more commonly seen in the emergency department. Many of guidelines are targeted to these patients. Determining when a patient can return to sports activities is a common question that providers need to prepare to answer. In 2010, the American Academy of Pediatrics (AAP) published basic concussion management guidelines for children and adolescents, adapted from the ICCS recommendations that emphasized a graduated return to play (RTP) protocol and the importance of having an athlete follow a stepwise progression in their RTP.
National Guideline/Academic Resources
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4004129/
References/Resources
Rozzelle CJ, Aarabi B, Dhall SS, et al. Management of pediatric cervical spine and spinal cord injuries. In: Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injuries. Neurosurgery 2013;72(Suppl 2):205-26.
Guidelines for the Management of Severe Head Injury. New York, NY: Brain Trauma Foundation 2000.
American Academy of Pediatrics. The management of minor closed head injury in children. Pediatrics 1999;104:1407-1415.
Mitchell KA, Fallat ME, Raque GH, et al. Evaluation of minor head injury in children. J Pediatr Surg 1994;29:851-854.
American Academy of Pediatrics Practice Guideline: The Management of Minor Head Injury in Children. Pediatrics 1999;104:1407-1415.
Lyttle MD, Crowe L, Oakley E, et al. Comparing CATCH, CHALICE and PECARN clinical decision rules for paediatric head injuries. Emerg Med J 2012;29:785-794.
Osmond MH, Klassen TP, Wells GA, et al. CATCH: A clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ 2010;182:341-348.
Kuppermann N, Holmes JF, Dayan PS, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: A prospective cohort study. Lancet 2009;374:1160-1170.
Bell MJ, Kochanek PM. Pediatric traumatic brain injury in 2012: The year with new guidelines and common data elements. Crit Care Clin 2013;29:223-238. PMID: 23537673.
Adelson PD, Bratton SL, Carney NA, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children and adolescents. Pediatr Crit Care Med 2003;4:S1-S75.
Adelson PD, Ragheb J, Kanev P, et al. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery 2005;56:740-754.
Hutchison JS, Ward RE, Lacroix J, et al. Hypothermia pediatric head injury trial investigators and the Canadian Critical Care Trials Group. Hypothermia therapy after traumatic brain injury in children. N Engl J Med 2008;358:2447-2456.
Curry R, Hollingworth W, Ellenbogen RG, et al. Incidence of hypo- and hyper-carbia in severe traumatic brain injury before and after 2003 pediatric guidelines. Pediatr Crit Care Med 2008;9:141-146.
Morris KP, Forsyth RJ, Parslow RC, et al. Intracranial pressure complicating severe traumatic brain injury in children: Monitoring and management. Intensive Care Med 2006;32:1606-1612.
Carter BG, Butt W, Taylor A. ICP and CPP: Excellent predictors of long-term outcome in severely brain injured children. Childs Nerv Syst 2008;24:245-251.
Wahlstrom MR, Olivecrona M, Koskinen L-OD, et al. Severe traumatic brain injury in pediatric patients: Treatment and outcome using an intracranial pressure targeted therapy – The Lund concept. Intensive Care Med 2005;31:832-839.
Catala-Temprano A, Claret Teruel G, Cambra Lasaosa FJ, et al. Intracranial pressure and cerebral perfusion pressure as risk factors in children with traumatic brain injuries. J Neurosurg 2007;106:463-466.
Figaji AA, Zwane E, Thompson C, et al. Brain tissue oxygen tension monitoring in pediatric severe traumatic brain injury. Part 1: Relationship with outcome. Childs Nerv Syst 2009;25:1325-1333.
Jagannathan J, Okonkwo DO, Yeoh HK, et al. Long-term outcomes and prognostic factors in pediatric patients with severe traumatic brain injury and elevated intracranial pressure. J Neurosurg Pediatr 2008;2:240-249.
Tintinalli JE, Kelen GD, Stapczynski JS, et al, eds. Tintinalli’s Emergency Medicine. 7th ed. New York: McGraw-Hill; 2011.
Pang D, Wilberger JE Jr. Spinal cord injury without radiographic abnormalities in children. J Neurosurg 1982;57:114.
Pang D. Spinal cord injury without radiographic abnormality in children, 2 decades later. Neurosurg 2004;55:1325.
Yucesoy K, Yuksel KZ. SCIWORA in MRI era. Clin Neurol Neurosurg 2008;110:429.
Patel JC, Tepas JJ 3rd, Mollitt DL, Pieper P. Pediatric cervical spine injuries: Defining the disease. J Pediatric Surg 2001;36:373.
Fesmire FM, Luten RC. The pediatric cervical spine: Developmental anatomy and clinical aspects. J Emergency Medicine 1989;7:133.
Mohseni S, et al. Effect of age on cervical spine injury in pediatric population: A National Trauma Data Bank review. J Pediatr Surg 2011;46:1771.
