Hospital Consult - September 2016
| Free Monthly News from Award Winning Publisher of: |
||||
| Hospital Access Manage- ment |
Hospital Case Manage- ment |
Hospital Employee Health | Hospital Infection Control | Hospital Peer Review |
| Health- care Risk Manage- ment |
Case Manage- ment Advisor |
IRB Advisor |
Medical Ethics Advisor |
Same- Day Surgery |
Mobile Technology May Ease ED Overcrowding
Reducing ED usage for routine care was a major goal of the Affordable Care Act. However, multiple recent reports show that contrary to expectations, ED visits are continuing to spike all across the country. ED overuse is a costly problem, in terms of direct costs and indirect damage. Long wait times cause frustration and complaints, which inevitably spill out on social channels and reflect on your hospital’s reputation.
Educating patients about alternative primary care can be challenge, however. Are patients aware of local options? With 66% of U.S. adults equipped with smartphones, leveraging mobile tools to manage ED traffic is a no-brainer. The following are app ideas ED providers can consider:
1. For patients arriving to the ED:
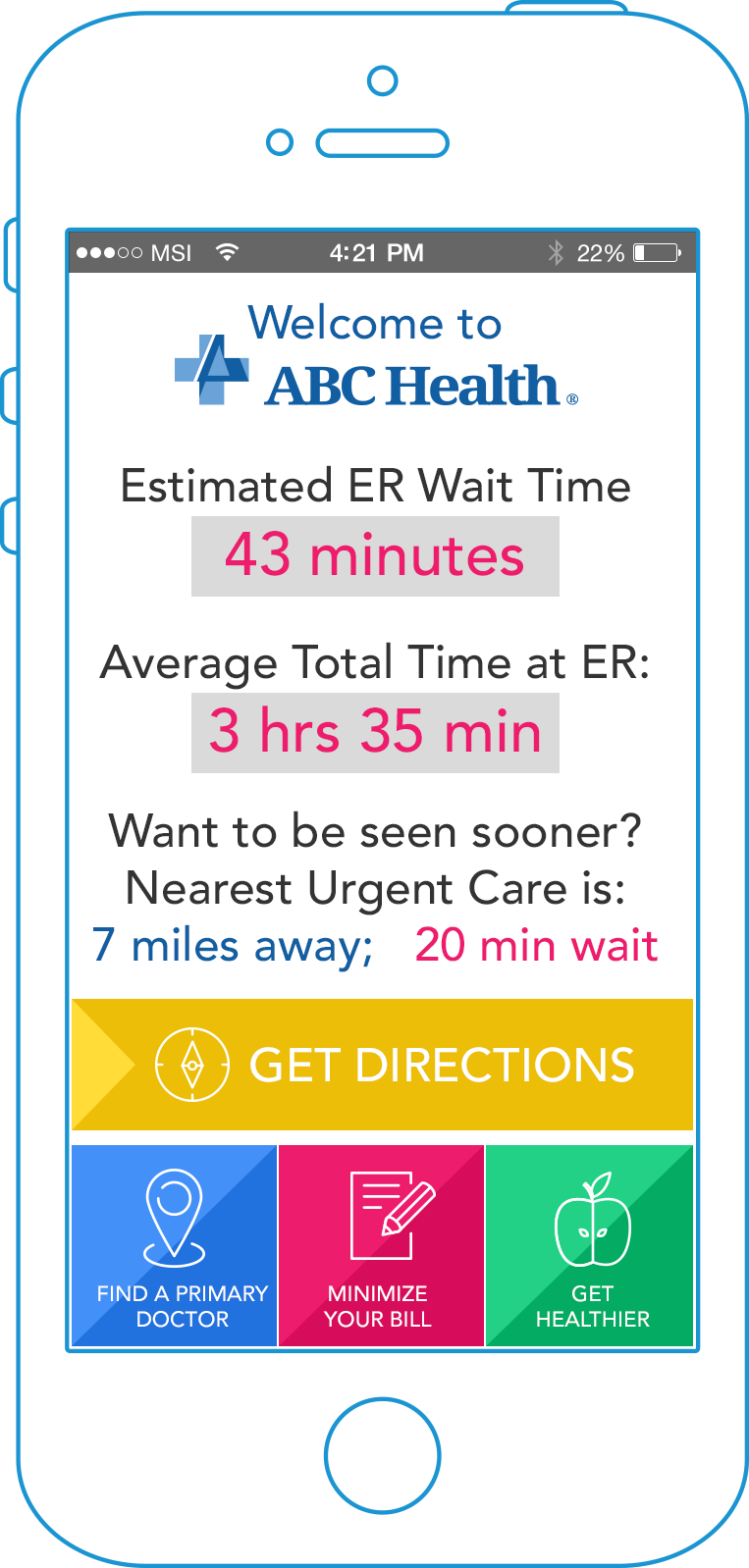
Offer visitors a simple ER app to view current wait times and the actual wait time post-triage. Patients can provide feedback directly from the app. This tells them: “We are listening, and we are keen to improve our service. Want to be seen sooner? View the nearest urgent care center; tap for GPS directions.”
Additionally, you can offer tips on how to minimize their bill. A user-friendly app explaining the financial effect of patients’ choices (copay vs. final bill, etc.) can encourage them to make responsible decisions.
2. For patients researching emergency care options:
Offer a branded urgent care app with easy search for in-network urgent care centers within proximity, with dynamically populated wait times. Allow patients to view common non-urgent conditions and symptoms. For example: “Do I need to go, or take my child, to the ED? Your app can help answer this question.”
Additionally, your app can send timely reminders for seasonal immunizations and wellness checks, advice regarding healthy habits, and more.
3. Engage super-utilizers:
If you have a group of “frequent flyers” visiting the ED for non-emergency problems, consider distributing an inexpensive smartphone with a pre-installed app. Enable patients to view overnight stay or primary care options within proximity, and see the face of their local primary care doctor.
For more tips on how to design these efficient mobile tools, and how to launch them quickly without breaking the bank, download the whitepaper: 12 Hospital Apps for Quick Mobile ROI – Reducing ER Overuse, Preventable Readmissions, Referral Leakage, and Physician Burnout.

Dangerous Practice for Hospitals: Releasing Patients with Unstable Vital Signs
DALLAS – Releasing hospitalized patients before all vital signs are stable is associated with an increased risk of death and readmission, yet the practice remains fairly common, according to a new report.
A study published recently in the Journal of General Internal Medicine finds that, at least in one large metropolitan area in the United States, 20% of patients were released from hospitals without fully stable vital signs.
Researchers from the University of Texas Southwestern Medical Center point out that, as hospital stays have contracted over the past 30 years, concerns have been raised that patients are being discharged too early. Noting the dearth of trials on the topic, the study team sought to determine if discharging patients with unstable vital signs actually leads to higher post-discharge mortality and readmission rates.
"We found that nearly 1 in 5 hospitalized adults is discharged with one or more vital sign instabilities such as an elevated heart rate or low blood pressure," said lead author, Oanh Nguyen, MD, Assistant Professor of Internal Medicine and Clinical Sciences. "This finding is an important patient safety issue because patients who had vital sign abnormalities on the day of discharge had higher rates of hospital readmission and death within 30 days even after adjusting for many other risk factors."
To determine that, researchers assessed electronic medical records of 32,835 unique individuals from six Dallas-Fort Worth area hospitals, recording abnormalities in temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation within 24 hours of discharge. They found that nearly 20% had one or more abnormalities, with elevated heart rate — which affected about 10% — the most common. Results also indicate that about 13% of those premature discharges were readmitted or died.
Patients with three or more instabilities had a nearly four-fold increase in the odds of death, study authors reported.
"Our findings, that 'vital signs are still vital,' have important implications for the development of national discharge guidelines to improve patient safety for the 35 million individuals being discharged from hospitals in the U.S. annually," said co-lead author Anil Makam, MD, Assistant Professor of Internal Medicine and Clinical Sciences.
"At a time when people are developing complicated, black box computerized algorithms to identify patients at high risk of readmission, our study highlights that the stability of vital signs, something doctors review with their own eyes every day, is a simple, clinically objective means of assessing readiness and safety for discharge. There's a good reason we call them vital signs," added senior author Ethan A. Halm, MD, general internal medicine chief at UT Southwestern. "It is important for clinicians to look at all of the vital signs in the 24 hours prior to discharge and not just the last set or the best ones in judging a patient's readiness for discharge."
Instead of current practices, study authors recommend that discharge guidelines include objective vital sign criteria for judging stability on discharge, which would improve disposition planning and post-discharge patient safety.
At a minimum, they advise, patients with one instability on discharge should be discharged with caution. Individuals with two or more instabilities should remain in the hospital for continued treatment and observation in the absence of extenuating circumstances, however.
In addition, hospitals are urged to provide close outpatient follow-up and appropriate patient education about warning signs and symptoms that call for urgent medical attention.
Furthermore, what appeared to be appropriate discharge planning wasn’t always good enough, according to study authors. Researchers found that patients sent to post-acute care facilities had still higher rates of readmission and death, suggesting that an alternate site of discharge might have been more appropriate for a significant subset of these individuals.

Ransomware Attacks Put Hospitals at Risk in a Variety of Ways
WASHINGTON, DC -- A recent federal interagency report indicates that, on average, 4,000 daily ransomware attacks have occurred since early 2016 — a 300% increase over the 1,000 daily ransomware attacks reported in 2015.
As if the possibility of a ransomware attack isn’t disturbing enough to hospital administrators, with medical facilities being among the most popular targets, an incident also could put the institutions in violation of HIPAA.
That information is contained in a new fact sheet provided by the U.S. Department of Health and Human Services (HHS). The document defines ransomware as a technique to exploit human and technical weaknesses to gain access to an organization’s technical infrastructure in order to deny the organization access to its own data by encrypting that data.
On the other hand, HHS provides reassurance of measures known to be effective to prevent the introduction of ransomware and to recover from a ransomware attack.
“This document describes ransomware attack prevention and recovery from a healthcare sector perspective, including the role HIPAA has in assisting HIPAA-covered entities and business associates to prevent and recover from ransomware attacks, and how HIPAA breach notification processes should be managed in response to a ransomware attack,” according to the fact sheet introduction.
The information is structured in a question-and-answer format. For example, in answer to the question, “What is ransomware?” the following answer is provided: “Ransomware is a type of malware (malicious software) distinct from other malware; its defining characteristic is that it attempts to deny access to a user’s data, usually by encrypting the data with a key known only to the hacker who deployed the malware, until a ransom is paid. After the user’s data is encrypted, the ransomware directs the user to pay the ransom to the hacker (usually in a cryptocurrency, such as Bitcoin) in order to receive a decryption key. However, hackers may deploy ransomware that also destroys or exfiltrates data, or ransomware in conjunction with other malware that does so.”
The HHS document also includes some practical advice on topics such as detecting a ransomware attack while in progress. It suggests the following can be indicators:
- a user’s realization that a link that was clicked on, a file attachment opened, or a website visited may have been malicious in nature,
- an increase in activity in the CPU and disk activity for no apparent reason (due to the ransomware searching for, encrypting and removing data files),
- an inability to access certain files as the ransomware encrypts, deletes, and renames and/or relocates data, and
- detection of suspicious network communications between the ransomware and the attackers’ command and control server(s). This would most likely be detected by IT personnel via an intrusion detection or similar solution.
The immediate response by a hospital should be to activate its security incident response plan and isolate the infected computer systems in order to halt propagation of the attack, according to the fact sheet. It also recommends that the local FBI or Secret Service field office be notified.
In terms of recovering from a ransomware attack, the federal agency states that, because ransomware denies access to data, maintaining frequent backups and ensuring the ability to recover data from backups is crucial to recovering from a ransomware attack.
HHS recommends that test restorations should be periodically conducted to verify the integrity of backed-up data and provide confidence in an organization’s data restoration capabilities.
“Because some ransomware variants have been known to remove or otherwise disrupt online backups, entities should consider maintaining backups offline and unavailable from their networks,” the document continues.
In fact, it says, implementing a data backup plan is a Security Rule requirement for HIPAA-covered entities and business associates as part of maintaining an overall contingency plan.
Based on HIPAA requirements, the fact sheet says hospitals and other facilities also should have processes to conduct post-incident activities, which could include a deeper analysis of the evidence to determine if any regulatory, contractual, or other obligations exist as a result of the incident and incorporating any lessons learned into the overall security management process to improve incident response effectiveness for future security incidents.
Part of that analysis would be assessing whether there was a breach of protected health information, which could be an impermissible disclosure that violates the Privacy Rule.

More Care Provided by RNs Can Reduce Hospital Restraint Usage
KANSAS CITY, MO – Many hospitals consider physical restraint an unnecessary evil. The problem is that these devices, such as belts, mittens, vests, bedrails, and geriatric chairs to restrict patients' freedom of movement to prevent them from hurting themselves or disrupting medical equipment and treatment, also can lead to agitation, confusion, adverse psychological effects, and pressure ulcers.
In the worst cases, the practice can even lead to strangulation and death.
Now, a new study appearing in the Journal of General Internal Medicine offers a solution: proper nurse staffing.
Researchers led by Vincent Staggs, PhD, of Children's Mercy Hospital and the University of Missouri-Kansas City, evaluated information collected on 869 hospitals providing care to more than 923,000 patients, as available in the National Database of Nursing Quality Indicators (NDNQI) between 2006 and 2010. Among information gathered by the NDNQI is quarterly data on restraints and monthly information on nurse staffing provided voluntarily by acute care hospitals.
Two nurse staffing variables were considered: staffing level (total nursing hours per patient day) and nursing skill mix (proportion of nursing hours provided by RNs). Outcomes were any use of restraint, regardless of reason, and use of restraint for fall prevention.
While use of restraints overall fell about 50% over the study period, results indicate that 1.6% of patients were restrained, about half of the time for the reported reason of preventing falls.
Researchers also were able to determine that the higher the average percentage of registered nurses on a shift, the less likely it was that restraint would be used. When a unit's percentage of registered nurses was low or very low relative to the unit's average, the odds of restraint were 11% and 18% higher, respectively, and the odds of fall prevention restraint were 9% and 16% higher.
Study authors suggest that the proportion of nursing care provided by the registered nurses rather than the total staffing level appears to be the more important predictor of restraint use.
"The findings suggest that patient care quality may suffer when unit staffing models cannot respond to changes in patient volume or registered nurse availability except by increasing the hours of staff who are not registered nurses," Staggs explained in a Springer press release. "This is further evidence that the type of nursing staff, not just the number of staff per patient, can be important for patient outcomes."
Having an adequate proportion of RNs, on the other hand, could reduce the likelihood of nursing staff requesting an order for restraint from a physician.
Staggs posits that the reason might be that registered nurses are better trained to find alternatives to restraint, adding, "In any case, restraint involves both nurses and physicians, and reduction in restraint use must be a collaborative effort.”

Overuse of ICU Often Means Lower Quality Care for Cardiovascular Patients
ANN ARBOR, MI – ICUs can literally be life-savers for patients who need them.
On the other hand, heart attacks or flare-ups of congestive heart failure can be treated elsewhere in the hospital — and probably should be whenever possible, according to a new study suggesting such patients fare worse in hospitals that rely heavily on ICUs to care for them.
The report, published recently in the journal CHEST, found that patients with those conditions in the ICU might be half as likely to get certain proven tests and treatments, and also be at much greater risk of dying a month after their hospital stay.
The University of Michigan Medical School-led researchers find that, in terms of cardiovascular care, hospitals sending the highest percentage of admits to the ICU perform worst on overall quality measures. Those conclusions were based on review of Medicare records from more than 570,000 hospital stays that took place in 2010.
Of the more than 150,000 hospitalizations at nearly 1,700 hospitals for acute myocardial infarction (AMI), 46% included care in an ICU. At the same time, 16% of the more than 400,000 hospitalizations for heart failure also included an ICU stay at one of 2,199 hospitals.
Hospitals were ranked on use of ICU and care quality based on the federal government's Hospital Compare website.
"In this country, we still have an open question of what to use the ICU for, and when, and very little evidence to guide physicians," explained lead researcher Thomas Valley, MD, MSc. "Is it for those who were already sick and got worse, or is it a place to send people proactively when we think they might get sicker? And the answer can vary on different days, or based on how many beds are available right then. We hope to build a body of evidence about how to use this valuable resource in the most effective way."
Hospitals treating fewer cases of AMI and heart failure also were the most likely to admit those patients to the ICU, as were for-profit hospitals.
Hospitals in the lowest quintile of ICU admission rates sent less than 29% of AMI and less than 8% of heart failure patients to ICUs. Hospitals in the top quintile, however, had rates of greater than 61% for AMI or more than 24% for heart failure.
Hospitals in the highest quintile had higher process measure failure rates for some, but not all, process measures, and also had greater 30-day mortality: 14.8% vs. 14.0% for AMI, and 11.4% vs. 10.6% for heart failure. Still, no differences were detected in 30-day readmissions or Medicare spending when compared to hospitals in the lowest quintile.
“Hospitals with the highest rates of ICU admission for patients with AMI or HF delivered lower quality of care and had higher 30-day mortality for these conditions,” the study authors concluded. “High ICU use hospitals may be targets to improve care delivery.”

| UPCOMING HOSPITAL WEBINARS Live Webinars Now Discounted 15% Or More! |
||
|---|---|---|
 |
Discharge Planning: CMS Worksheet & Standards | Sign Up → |
 |
Violence Prevention in Healthcare: OSHA Requirements | Sign Up → |
 |
Transitions in Care and the Bundled Payment Population | Sign Up → |
 |
Hospital CMS CoPs Made Easy: The Series – Part II | Sign Up → |
 |
Hospital CMS CoPs Made Easy: The Series – Part III | Sign Up → |
 |
Hospital CMS CoPs Made Easy: The Series – Part IV | Sign Up → |
 |
Case Management in Acute Care and Community-Based Settings | Sign Up → |
 |
Hospital CMS CoPs Made Easy: The Series – Part V | Sign Up → |
 |
Case Management Best Practices: Communication & Hand-Offs | Sign Up → |
 |
Interdisciplinary Rounding to Improve Case Management Outcomes | Sign Up → |
 |
Prioritize Patient Needs at Every Level | Sign Up → |