Who Needs an Endometrial Biopsy?
By Rebecca H. Allen, MD, MPH
Associate Professor, Department of Obstetrics and Gynecology, Warren Alpert Medical School of Brown University, Women and Infants Hospital, Providence, RI
Dr. Allen reports she is a Nexplanon trainer for Merck, and has served as a consultant for Bayer and Pharmanest.
SYNOPSIS: In this retrospective cohort study of premenopausal women with abnormal uterine bleeding, obesity, as opposed to age, was the most significant predictor of complex hyperplasia or cancer on endometrial biopsy.
SOURCE: Wise MR, Gill P, Lensen S, et al. Body mass index trumps age in decision for endometrial biopsy: Cohort study of symptomatic premenopausal women. Am J Obstet Gynecol 2016;215:598.e1-8.
This is a retrospective cohort study conducted in New Zealand from 2008 to 2014. Women were included if they were 55 years of age or younger, had a history of abnormal uterine bleeding, were not menopausal (either by history, or amenorrhea ≥ 6 months, or serum follicle-stimulating hormone level > 20 IU/L), and underwent an endometrial biopsy. Exclusions were women with a known history of endometrial cancer or complex hyperplasia before 2008. The primary outcome was the histologic diagnosis of complex hyperplasia, complex atypical hyperplasia, or endometrial cancer. Data were collected from the medical record, including measured height/weight within one year of the biopsy, age, parity, menstrual history, medical history, family history of cancer, socioeconomic status, and use of hormone therapy. Hemoglobin, pelvic ultrasound, and hysterectomy results also were recorded, if performed.
A total of 916 women met the inclusion and exclusion criteria. Half (n = 451) of the women had a body mass index (BMI) ≥ 30 kg/m2, and 85% of the subjects underwent Pipelle endometrial biopsy, 22% had sharp curettage (presumably a dilation and curettage in the operating room), and 7% had both. The mean age was 43.7 ± 6.4 in the non-obese group and 42.0 ± 7.2 in the obese group. Of 840 women with sufficient tissue for diagnosis, 41 (4.9%) women were diagnosed with endometrial hyperplasia with or without atypia or cancer. In univariate analysis, women of Indian and Pacific ethnicity had a higher odds of having complex hyperplasia or cancer compared to European women (odds ratio [OR], 6.21; 95% confidence interval [CI], 2.11-18.32). However, this variable was confounded by the fact that 92% of the women of Indian and Pacific ethnicity were obese; therefore, BMI was chosen for the multivariate model because it was more generalizable and biologically plausible. Other variables associated with the outcome were nulliparity (OR, 2.51; 95% CI, 1.25-5.05), anemia (OR, 2.38; 95% CI, 1.25-4.56), and thickened endometrium on ultrasound (OR, 4.04; 95% CI, 1.69-9.65). In the multivariable analysis, after adjusting for age, anemia, and nulliparity, obese women had higher odds of having complex hyperplasia or cancer compared to non-obese women (adjusted OR, 4.00; 95% CI, 1.36-11.74), while overweight women showed no increased risk. Nulliparity and anemia remained significant predictors in the multivariate model.
COMMENTARY
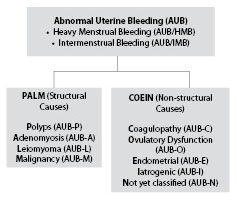
Abnormal uterine bleeding (AUB) is one of the most common reasons for referral to the gynecologist and is divided into heavy menstrual bleeding and intermenstrual bleeding. The cause of AUB is classified by the PALM-COEIN terminology. (See Figure 1.) The decision whether to perform an endometrial biopsy to rule out endometrial hyperplasia or cancer is informed by clinical factors. Risk factors for endometrial cancer include age, obesity, nulliparity, infertility, late-onset menopause, diabetes, and hypertension. The number of new cases of endometrial cancer in the United States was 25.4 per 100,000 women per year in 2013.1 The American College of Obstetricians and Gynecologists recommends endometrial biopsy as afirst-line test in women age 45 and older.2 For younger women, it recommends that biopsy be performed in those with a history of unopposed estrogen (as in obesity or polycystic ovary syndrome), failed medical management, and persistent abnormal uterine bleeding. The National Institute for Health and Care Clinical Guideline on heavy menstrual bleeding in the United Kingdom recommends a biopsy in women with persistent intermenstrual bleeding, women aged 45 and older, or those experiencing treatment failure.3 This study reported on the strong role of obesity as a risk factor and recommends changing guidelines to reflect its prominent influence on the development of endometrial hyperplasia and cancer.
Figure 1: Abnormal Uterine Bleeding (AUB) |
 |
The main clinical question is: how many endometrial biopsies must be performed in premenopausal obese women with abnormal uterine bleeding to detect one case of endometrial hyperplasia or cancer? In the current study, there were 12 (1.4%) cases of endometrial cancer, nine (1.1%) cases of complex hyperplasia with atypia, and 20 (2.4%) cases of complex hyperplasia without atypia. Among obese women, 31 of 451 (7.4%) were diagnosed with endometrial hyperplasia or cancer compared to four of 208 (1.9%) overweight women and six of 257 (2.3%) normal weight women. The authors didn’t calculate a “number needed to screen” to detect a case of endometrial hyperplasia or cancer. Nevertheless, we currently have a blanket recommendation to screen all women age 45 years and older for endometrial hyperplasia or cancer if they present with abnormal uterine bleeding. The reasoning behind this age cutoff is that 1.6% of all endometrial cancer cases occur among women 20-34 years of age, 5.4% between the ages of 35-44 years, and 17.2% occur among women 45-54 years of age, with the remainder occurring at older ages and a median age of diagnosis of 62 years. Nevertheless, I definitely see the logic of using BMI as an additional risk stratification measure in younger women, with a BMI ≥ 30 kg/m2 prompting an endometrial biopsy in women with abnormal uterine bleeding. In this way, even if endometrial hyperplasia rather than cancer is diagnosed, we actually have the opportunity to prevent progression to cancer with progestin treatment or hysterectomy, depending on the clinical circumstances.
REFERENCES
- National Cancer Institute. SEER Stat Fact Sheets: Endometrial Cancer. Available at: https://seer.cancer.gov/statfacts/html/corp.html. Accessed Dec. 1, 2016.
- ACOG Practice Bulletin Number 128. Diagnosis of Abnormal Uterine Bleeding in Reproductive-Aged Women. July 2012.
- National Institute for Health and Care Excellence (NICE). Heavy menstrual bleeding: Assessment and management. Clinical Guideline 44. Available at: https://www.nice.org.uk/guidance/cg44. Accessed Dec. 1, 2016.
In this retrospective cohort study of premenopausal women with abnormal uterine bleeding, obesity, as opposed to age, was the most significant predictor of complex hyperplasia or cancer on endometrial biopsy.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
