Acute Trauma Care in the Era of SARS-CoV-2
March 1, 2022
Reprints
AUTHORS
Melanie Sich, Medical Student, Wright State University Boonshoft School of Medicine, Dayton, OH
Vincent Marsh, MD, Associate Professor of Emergency Medicine, Wright State University, Dayton, OH
PEER REVIEWER
Dennis Hanlon, MD, FAAEM, Vice Chairman, Academics, Department of Emergency Medicine, Allegheny General Hospital, Pittsburgh
EXECUTIVE SUMMARY
- Hospital-transmitted SARS-CoV-2 has been a significant problem, with reports of approximately 4.9% of hospitalized or admitted patients being identified as “COVID nosocomial-infected patients” in some studies.
- Mortality has been associated with certain health conditions, including age older than 60 years, male gender, smoking history, obesity, preexisting pneumonia, and significant comorbid illnesses, including immunocompromised states, diabetes mellitus, and cardiovascular, cerebrovascular, pulmonary, and kidney diseases.
- Interestingly, there seems to be some radiographic overlap between pulmonary contusions and early COVID-19 infections, which may be aided by computed tomography imaging to help differentiate the former from the latter. The distinguishing features of pulmonary contusions are focal, non-segmental areas of parenchymal opacification in the peripheral lung field. Meanwhile, those for the early phase of COVID-19 are bilateral ground glass opacities within subpleural areas (sometimes referred to as “crazy paving pattern”) later replaced by more definitive consolidation.
COVID-19 has affected every aspect of medical care. The authors discuss modifications of the care of trauma patients to protect both patients and providers.
— Ann M. Dietrich, MD, Editor
Introduction
A previously unknown SARS-CoV-2 (COVID-19) virus was first detected in Wuhan, China, in December 2019 after a significant outbreak of unusual respiratory illnesses. Spreading rapidly, the viral illness was later declared a global health emergency by the World Health Organization. Both the virus and the public health measures have greatly affected global healthcare systems. Hospital infrastructure and resources have been overwhelmed by increasing COVID-19 cases, while the frequency, severity, and clinical presentations of traumatic injuries have changed. The new obstacles facing trauma care workers have primarily revolved around the need for increased protection against viral transmission and an ever-present shortage of resources.
The SARS-CoV-2 virus is known to spread between human hosts via respiratory droplet exposure to mucosal surfaces. Hospital-transmitted COVID-19 has been quite problematic throughout the pandemic, often stemming from common aerosol-generating procedures, such as intubation. Emergency/trauma physicians, nurses, and providers must be able to anticipate the potential risks of typical trauma management techniques and procedures, bypassing the dangerous steps when possible, to protect themselves and their patients. To accomplish this, experts have developed a variety of guidelines and recommendations for modifying trauma care in the era of COVID-19, which are summarized in this article.
This article provides a brief overview of the definition, pathophysiology, clinical features, and epidemiology of SARS-CoV-2 and its impact on trauma care, including novel approaches to reduce spread among patients and providers. Further discussion includes the need for infection control, guidelines for appropriate use of personal protective equipment (PPE), and proposed restructuring of the trauma bay to mitigate cross-infection risks. Additionally, a summary of COVID-19 screening guidelines in the trauma setting are provided. Finally, challenges to airway management, ventilatory support, resuscitation, and high-risk procedures in the era of COVID-19 are discussed, as well as new surgical triage processes, anesthetic recommendations, and preoperative, intraoperative, and postoperative precautions.
Pathophysiology, Clinical Features, and Epidemiology
In an emergency healthcare setting, the term trauma refers to an acute injury leading to tissue destruction from an accident or act of violence via mechanical, chemical, thermal, or electrical means.1 The management of trauma patients has evolved over time, leading to a highly systematic process of evaluation. This affords providers the opportunity to rapidly assess and respond to a plethora of differing injury patterns across multiple patient populations. With most trauma presentations, large amounts of resources are mobilized and directed toward the primary and secondary surveys of trauma in the hopes of mitigating morbidity and mortality. However, beginning early in 2020, trauma management and resource use was affected greatly by the COVID-19 pandemic.
In December 2019, a series of unprecedented novel coronavirus infections emerged within the Wuhan province of China, leading to a significant outbreak of respiratory illnesses.2 Furthermore, rapid transmission evidenced by an R0 between 1.4 and 3.9 led to its spread across multiple countries and, ultimately, the SARS-CoV-2 pandemic.3 The SARS-CoV-2 virus has been found to spread via human-to-human respiratory droplets through sneezing, coughing, and talking, and indirectly via contaminated objects.2 The exposure of the respiratory droplets to the recipient’s mucosal surfaces (eyes, nose, or mouth) allows for transmission of the pathogen.4 Fomites (bedsheets, blankets, utensils, etc.) and fecal-oral transmission have been documented on fewer occasions.2,4 Importantly, hospital-transmitted SARS-CoV-2 has been a significant problem, with reports of approximately 4.9% of hospitalized or admitted patients being identified as “COVID nosocomial-infected patients” in some studies.4 Airborne transmission of SARS-CoV-2 has played a lesser role in transmission except in circumstances in which large amounts of aerosols are generated, such as with endotracheal intubation, bronchoscopy, pneumothorax management, etc.4
COVID-19 is associated with a wide spectrum of clinical severity, ranging from asymptomatic to severe infections.2 In approximately 20% of COVID-infected patients, the disease progresses to severe respiratory manifestations in need of acute treatment, with 14% of patients developing severe pneumonia and close to 5% developing acute respiratory distress syndrome (ARDS), sepsis, or multisystem organ failure.5 The most common presenting symptoms include fever, cough, shortness of breath, malaise, weakness, loss of taste and smell, and digestive symptoms.2
Mortality has been associated with certain health conditions, including age older than 60 years, male gender, smoking history, obesity, preexisting pneumonia, and significant comorbid illnesses, including immunocompromised states, diabetes mellitus, and cardiovascular, cerebrovascular, pulmonary, and kidney diseases.4 Clinically significant infection rates in the 0-19-year age group have been low and have presented predominantly with mild symptomatology.4
In response to the COVID-19 pandemic, governments around the world organized “lockdowns” enacting social restrictions, thereby attempting to limit the virus’s spread.6 Importantly, initial public health recommendations advised patients to avoid unnecessary healthcare utilization to minimize viral transmission and to maintain hospital capacity to accommodate expected surges of COVID-infected patients.7 These public health measures altered access to healthcare and thereby altered systemic healthcare delivery.8 Despite public health measures, traumatic injuries remained a reality, and patients continued to require healthcare resources amid a raging pandemic. However, the incidence of cases, mechanism, severity, and timing of presentation were altered dramatically.8 These changes ultimately resulted in a marked redistribution of medical resources to meet demand.8 One study found that the incidence of emergency medical services (EMS) calls was reduced by 12%, with a 23% reduction in trauma-related calls during the lockdown period.9 Moreover, the United States, along with several other countries, experienced sharp declines in emergency department (ED) visits during the peak of social restrictions in April 2020. Multiple studies estimated a decline in ED visits of 22% to 57.4% in adults and by 70% in the pediatric population.6,7,10-15 Trauma-related ED visits in particular decreased by approximately 30% to 52.7%, and trauma patients who did present to the ED generally had more severe injuries and endured longer intensive care unit (ICU) stays when compared to pre-pandemic cases.8,11,16
Additionally, many studies have highlighted the role public health measures played in altering the nature of traumatic injuries, both qualitatively and quantitively.6,7,10-15 For example, motor vehicle collision injuries substantially decreased by greater than 80% along with sports-related injuries, many of which were prevented secondary to social restrictions requiring avoidance of travel and outdoor group activities.8,15 However, despite the absolute decrease in trauma presentations during the lockdown periods, a shift toward increased interpersonal violence was seen. Multiple studies found the incidence of penetrating traumas doubled, with marked increases in assaults, domestic violence, and high-energy falls, especially in the pediatric population.6,8,15 Social isolation also affected rates of alcohol and drug abuse, resulting in proportional increases in opioid overdoses presenting to EDs.9,10,17 Additionally, trauma patients admitted during the lockdown period were found to have higher rates of drug and alcohol use.17 This is significant, since patients with substance abuse have been found to have a nine-fold increase in contracting COVID-19 and have higher mortality and complication rates associated with their COVID-19 infections.17
Trauma Care Limitations Imposed by COVID-19
The threat of cross-infection as well as resource scarcity have played a major role in precipitating healthcare changes. Hospital-acquired COVID-19 has been a serious problem from the outset of the pandemic: An early study found that almost one-third of China’s COVID-infected population consisted of healthcare workers whose infections were traced back to the healthcare setting.18 As trauma patients often receive care in multiple settings, such as the ED, the operating room (OR), and/or ICUs, their contact with multiple people, objects, and equipment magnifies the risk of viral transmission and may be especially difficult to avoid.19 In addition to restructuring the trauma bay and reimagined triage strategies, PPE has been essential to mitigating the risks of transmission both among patients and healthcare workers.19
Additionally, a shortage of PPE, such as N95 masks, sterile gowns, and gloves, and a shortage of negative pressure rooms have made treating patients even more challenging during the pandemic.20 A lack of PPE not only endangers patients and healthcare workers, but it also limits manpower and personnel actively involved in patient resuscitations.20 Moreover, the increasing number of hospitalized COVID-positive patients has reduced surgical capabilities, including the number of available surgical suites, available post-operative beds, and specific resources such as oxygen, ventilators, medications, etc., that are reallocated for COVID-infected patients.21 Early in the pandemic, hospitals around the world declared a state of emergency due to the depleting resources, and it became evident that previously established best practices would no longer be possible.21 The main challenge for hospitals since then has been to balance patient-centered care, staff safety, and the optimal use of limited resources among an unrelenting pandemic.
Given the finite supply of resources and the ongoing COVID-19 pandemic, the Centers for Disease Control and Prevention (CDC) has developed an approach to conserving PPE in hopes of limiting supply shortages while attempting to protect individuals from exposure risk. They recommend using respirators with an expired shelf life or those approved for occupational use if shortages are present; however, this is to be avoided in the surgical setting.22 Additionally, they call for the reusing of N95 masks or prioritizing the use of N95 masks and powered air purifying respirators (PAPRs) for the highest risk circumstances, including aerosol-generating procedures (AGPs).22 If no respiratory PPE is available, the CDC recommends designating healthcare personnel who have recovered from COVID-19 and/or who are fully vaccinated to be primary caregivers, while limiting care from those with increased risk of infection.22
Human Infection Control
According to the CDC, all healthcare interactions, regardless of infection status, require standard precautions to prevent disease spread, including proper hand hygiene, cleaning of supplies, disposal of waste, and appropriate sharps disposal.23 Additional measures are recommended to reduce viral particle transmission when interacting with COVID-positive/presumed positive patients. These include contact precautions, such as donning of PPE including gloves, gown, and protective eye wear, in addition to airborne precautions (properly fitted N95 respirator mask or a PAPR).23
The World Health Organization (WHO) recommends droplet and contact precautions for all healthcare staff working with patients with suspected or known COVID-19, while the CDC and the European Centre for Disease Prevention and Control (ECDC) recommend airborne precautions for all healthcare personnel in these situations.24,25 Moreover, the American College of Surgeons (ACS) recommends that all staff in the OR wear N95 respirators if possible, particularly when operating on confirmed COVID-19 cases.22 It also is recommended that enhanced droplet/airborne PPE be used during any AGPs.25 (See Figure 1.) Given the limited lead time and increased need for urgent/emergent care associated with traumatic injuries, many trauma patients are unable to undergo COVID-19 screening prior to initial evaluation. Thus, experts have recommended donning PPE under the assumption that trauma patients are COVID-positive until proven otherwise.22,26
Figure 1. An Example of Enhanced Droplet/Airborne PPE in Preparation for Intubation of a Patient with Suspected or Confirmed COVID-19 Incorporating the Use of a Fit-Tested N95 Mask
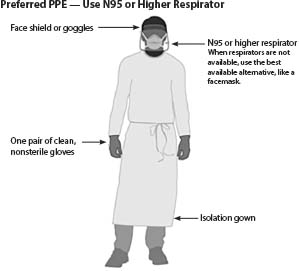
PPE: personal protective equipment
Source: Centers for Disease Control and Prevention
EMS and Prehospital Operation Strategies
EMS plays a key role in promptly triaging patients as well as providing timely and effective emergency care and transport to nearby healthcare facilities. It is recommended that EMS call centers should develop strategies to screen patients for SARS-CoV-2 infection before EMS arrives on scene to allow for adequate time to properly plan management strategies and don appropriate PPE. Ideally, callers should be queried about signs and symptoms of COVID-19 or recent exposures.27 However, the CDC states that this screening process should never supersede the communication of pre-arrival instructions (e.g., cardiopulmonary resuscitation [CPR]) if urgent lifesaving interventions are indicated.27
If a COVID-19 infection is not suspected in the patient (based on symptom and exposure risk potentially elicited during the 911 call or on scene), the CDC recommends that EMS personnel follow standard precautions in addition to eye protection and a facemask.27 If a patient is suspected of SARS-CoV-2 infection, however, an N95 respirator, gown, gloves, and eye protection along with standard precautions are warranted.27
Caution should be exercised in performing any AGPs, and all individuals involved should don an N95 respirator or equivalent during the process.27,28 The CDC advises that the rear doors of the ambulance be opened, and the heating ventilation and air conditioning (HVAC) system should be activated during these procedures if possible.27 Note that the presence of COVID-19 does not alter best-practice techniques associated with CPR because it is an essential lifesaving measure.28 However, as mentioned earlier, appropriate steps should be taken to mitigate viral transmission. Responders may consider modifying resuscitation choreography, for example, positioning additional rescuers away from the immediate resuscitation area to reduce the chances of rescuer exposure.28 However, such new techniques should only be executed after proper training, since such strategies have the potential to create delays or interruptions in CPR.
When transport to a nearby healthcare facility is needed, EMS responders should make sure to notify the facility of any suspected or confirmed COVID-19 patients to allow for appropriate infection control precautions prior to the patient’s arrival.27 When possible, the CDC advises that ambulance ventilatory system be placed in the nonrecirculation mode during transportation and also recommends the use of the rear exhaust fan to draw air way from the cab and out the back end of the vehicle.27 EMS personnel should continue to wear a facemask and eye protection, at a minimum, when arriving with patients to the healthcare facility.27
Environmental Infection Control
In the setting of the COVID-19 pandemic, it is essential for trauma centers to redesign patient triage areas and healthcare delivery areas with readily available supplies, easy access to PPE, and appropriate staffing.18,29 Many hospitals around the world have been implementing a “hot/warm/cold” zone approach to separate areas by degree of exposure risk. They also call for the designation of specific roles for each zone to minimize viral spread and resource over-utilization.3,19,26 The hot zone includes a three-foot, clearly demarcated border around the trauma patient, and it is considered to be potentially contaminated.19,26 Adjacent to this zone is the warm zone, which is used for transferring supplies from cold to hot zones as well as for donning and doffing PPE.19,26 The cold zone is a designated area for available supplies and staff who are not involved in resuscitation.19,26 It is recommended that any patient who is suspected to be COVID-positive be placed immediately in an airborne isolation room (single, negative pressure room with frequent air exchange) or at least a single room with closed doors if possible.30
Approach to Trauma Patient
Upon initial arrival to the ED, it is recommended that all patients, regardless of symptoms, wear facemasks if possible.29 All should be assumed to be COVID-positive on initial arrival until further assessment is completed.19 While patients with major trauma should be admitted for immediate stabilization/surgical intervention, minor trauma patients should undergo COVID-19 screening procedures prior to admission to the hospital.19 Initial screening includes obtaining a history from the patient, including details about any exposures, recent travel, or sick contacts, as well as COVID-19 symptoms (fever, cough, shortness of breath, or malaise).19,30,31 Patients generally are considered to be high risk if they are deemed to be COVID-19-positive via clinical evaluation and/or radiographic/serologic testing.22
Initial recommendations for testing include first obtaining a reverse transcriptase polymerase chain reaction (RT-PCR) respiratory swab sample, preferably from the nasopharynx.31 If the test results are negative but the provider has a high clinical suspicion for COVID-19, a repeat RT-PCR test is indicated, since this test has the potential to produce false-negative results. Some authorities initially recommended obtaining a computed tomography (CT) scan of the chest if suspicion is extremely high and tests are negative (most accurate radiological tool to confirm COVID-19 [98% sensitivity]), but this practice has come into question recently because it entails a large amount of resources, increased risk of viral spread, and increased radiation exposure to the patient.31
Alternatives include chest X-ray or point-of-care ultrasound (POCUS).31 It should be noted that COVID-19 screening and evaluation should not impede or slow the management of acute trauma patients. However, these screening recommendations should be employed in concert with trauma care when indicated.
Radiology
Because of the use of PPE, portions of the physical exam may be limited or incomplete.3 This may necessitate an increased reliance on radiographic testing for injury assessment. Some trauma centers also have found it helpful to establish a dedicated CT room in close proximity to the trauma bay to minimize travel within the hospital and, thus, reduce the risk of potential contamination and CT downtime for decontamination.19 Interestingly, there seems to be some radiographic overlap between pulmonary contusions and early COVID-19 infections, which may be aided by CT imaging to help differentiate the former from the latter.19 The distinguishing features of pulmonary contusions are focal, nonsegmental areas of parenchymal opacification in the peripheral lung field. Meanwhile, those for the early phase of COVID-19 are bilateral ground glass opacities within subpleural areas (sometimes referred to as “crazy paving pattern”) later replaced by more definitive consolidation.19
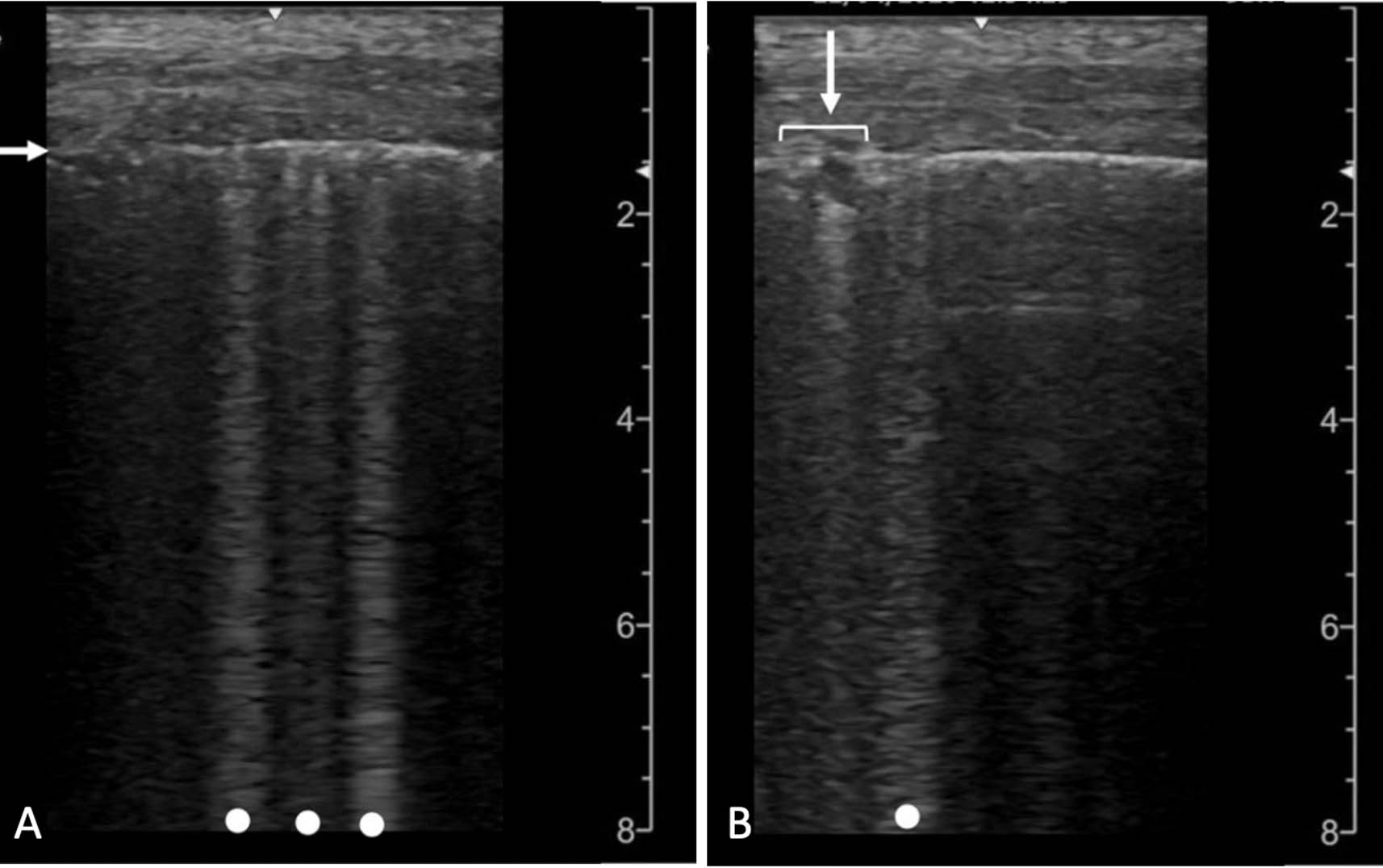
For rapid evaluation, especially in cases of limited radiological resources, POCUS has been demonstrated to be a helpful and effective tool for triage, risk stratification, and evaluation of lung disease progression.32,33 The most consistent and specific findings associated with COVID-19 on ultrasound evaluation are the coalescence of B-lines (Figure 2A) and pleural line defects (Figure 2B).32 Ultrasonography also has been reported to have higher sensitivity and specificity rates for conditions such as pneumothorax, pleural effusion, pneumonia, and congestive heart failure compared to a chest X-ray.32,33 Moreover, POCUS limits radiation exposure and allows for rapid interpretation of results, avoiding delays in further interventions.32,33
Figures 2A and 2B. Lung Ultrasound Findings Associated with COVID-19 |
Multiple B-lines (dots) are shown with irregularity of the pleural line (arrow) in (A). A small subpleural consolidation (arrow) is shown with a B-line (dot) in (B). Reprinted from: Kameda, T, Mizuma, Y, Taniguchi, H, et al. Point-of-care lung ultrasound for the assessment of pneumonia: A narrative review in the COVID-19 era. J Med Ultrasonics 2021;48:33. Open access, Creative Commons: https://creativecommons.org/licenses/by/4.0/ |
Airway Management, Ventilatory Support, Resuscitation
Airway management and resuscitation have become an even more challenging aspect of trauma care in the era of COVID-19. They typically involve risky AGPs, such as intubation, airway suctioning, noninvasive ventilation, bronchoscopy, chest tube insertion, and tracheostomy formation, to name a few. These, along with other high AGPs, are thought to be responsible for a large majority of healthcare SARS-CoV-2 transmissions.19,30,31 Table 1 provides a list of AGPs considered by the CDC to be high risk.25 These procedures must be approached with special caution. Ideally, they all should be performed in an airborne isolation room with a limited number of personnel who each don appropriate airborne/droplet PPE, including N95 respirators or PAPR.30 The healthcare team member with the most experience should be designated to perform the procedure, with the goal of optimizing first-attempt success and, thus, reducing exposure to aerosolization of respiratory secretions.19,34
Table 1. Risk Consideration for Resuscitation Procedures During the COVID-19 Pandemic | |
Aerosol-Generating Procedures* |
PPE Recommendations for Aerosol-Generating Procedures Performed on COVID-19 Patients |
|
|
* Current list provided by World Health Organization Source: Centers for Disease Control and Prevention | |
Intubation
The patient’s torso should be slightly elevated to optimize his or her position in preparation for preoxygenation and airway management. Hypoxemic patients who need emergency intubation may not be able to tolerate lying flat.35 Elevated positioning, also known as ramping, improves ventilation/gas exchange and additionally helps to reduce atelectasis in dependent lung tissue, especially among obese patients. Ear to sternal notch positioning also improves respiratory mechanics and increases visualization during direct laryngoscopy. However, these positioning techniques may be limited by the need to ensure spinal immobilization. Providers should prepare themselves with the use of proper high-level PPE as well as the use of double gloves (outer pair to be removed after laryngoscopy).36
Previous guidelines have encouraged the use of rapid sequence induction (RSI) for confirmed or suspected COVID-19 patients, since this technique is designed to minimize the chance of aerosol generation from mask ventilation and improve the first-pass success rate.35 However, newer research has suggested that uncomplicated mask ventilation may not produce significant aerosol generation.37 Unique patient factors should be considered when deciding whether to perform an RSI-facilitated intubation. It is important to anticipate the physiologic effects of RSI on critically ill patients. While RSI increases first-pass success rates, it also has the potential to increase hypoxemia and hypotension after induction and during intubation.38 For this reason, some experts recommend delayed sequence intubation or paralytic-free intubation in those at the highest risk of decompensation. They also recommend pre-oxygenation with 100% FiO2 and appropriate resuscitation prior to intubation if hemodynamics and/or other clinical factors permit.38,39 This may be accomplished with a tight-fitting facemask, high flow nasal cannula with an overlying surgical mask, and even noninvasive positive pressure ventilation (NIPPV), such as continuous positive airway pressure (CPAP) in the right clinical context. In instances when facemask ventilation use is necessary, it is recommended that low volume, low pressure breaths are performed.38,39
Clinicians are encouraged to use video laryngoscopy (VL) during intubation because it increases first-pass success rates in patients in whom a difficult airway is anticipated. It also is the recommended laryngoscope in the context of spinal immobilization since its hyper-angulated blade helps to overcome the limitations of positioning in these patients.30 Moreover, it positions the clinician at a greater distance from the patient’s oropharynx during the procedure.19 However, if VL is not available, or if it is a modality the clinician is not familiar with, it is recommended that they use direct laryngoscopy (DL).19,30 Additionally, in the setting of a difficult airway (e.g., maxillofacial or cervical spine trauma), experts recommend avoiding awake fiberoptic intubation unless absolutely necessary.3 This modality increases the likelihood of oropharyngeal irritation and, thus, may increase coughing and aerosol generation. If awake intubation must be performed, effective airway anesthesia should be achieved with the use of nerve blocks and/or topical local anesthetic.35,40 However, nebulized local anesthetics or transtracheal local anesthetic injections should be avoided because of their risks of aerosol generation.30
Once intubation is complete, experts advise against the use of auscultation when seeking to confirm proper positioning of the endotracheal tube in a suspected or confirmed COVID-19 patient. They suggest using end-tidal carbon dioxide (EtCO2), examining for equal chest rise, radiography and/or using POCUS for guidance.35,36,41
Once tube positioning is confirmed, the cuff should be inflated prior to ventilator connection.35 Clinicians should ensure there is no leak around the cuff after giving a breath. A closed suction system may be used as necessary for tracheal/oral suctioning before extubation.40 Experts advise that a high efficiency particulate air (HEPA) viral filter be present with the suctioning equipment. The following are recommendations for lung protective mechanical ventilation strategies postintubation: target tidal volume 6 mL/kg predicted ideal body weight, plateau pressure ≤ 30 cm H2O, target SaO2, 88% to 95%, and pH ≥ 7.25.30
Several techniques have been proposed for decreasing viral spread during extubation. Some have recommended the use of cough prophylaxis: lidocaine, low-dose opioids, or dexmedetomidine.35 To prevent spread of secretions, a surgical mask may be placed on the patient while the endotracheal tube is still in place.35 If the patient begins to cough, it is recommended that wet gauze be placed over the patient’s nose and mouth prior to extubation.40 An alternative option is to shield the patient’s face with a clear plastic drape. A surgical mask should be placed over the patient’s airway after extubation with supplemental oxygen as needed.35 Additionally, it should be noted that initial recommendations called for the use of protective barrier enclosures (usually in the form plexiglass cubes or domes) for high-risk intubations.42 These barriers provided operators with increased protection from aerosols, since they encapsulated the patient’s head and neck in a see-through barrier. Operator ports were available, which allowed for the passage of equipment and permitted access to conduct the intubation. Although aerosol transmission was reduced with the use of protective barrier enclosures, their restrictive nature led to increased intubation times and degradation of first-pass success. Given these constraints, experts have recommended against the use of protective barrier enclosures during intubation when appropriate PPE is available.42
Cricothyrotomy
In the event that intubation fails or is not feasible (airway blockage from traumatic face or neck injury), emergency providers may need to use alternative procedures. Specifically, the bougie-assisted surgical cricothyrotomy may be used in situations where neither oxygenation nor ventilation can be implemented effectively.43 Some experts have found that the use of wet OR towels as neck coverings has been an effective technique to suppress aerosolization during cricothyrotomy.43
Thoracostomy
Tube thoracostomy, commonly used in cases of traumatic hemothorax and/or pneumothorax, also may be a potential AGP.44 These procedures, as well as their tube drainage system, may pose a potential risk of viral spread, especially if an air leak exists in the system. To minimize potential viral aerosolization, it is recommended that the drainage system be set up prior to the procedure, with the additional recommendation of adding dilute bleach to the water seal chamber instead of water alone.44 The tube should be clamped prior to insertion, and ventilation should be held before entering the pleural space and until the tube is placed if it is safe for the patient.44 Digital confirmation is recommended to confirm tube entry into the thoracic cavity.44 Cable ties, instead of tape, should be used to ensure effective connection between the tube and drainage system.44 Additional sutures are recommended when closing the skin incision as an additional precaution to prevent air leaks.44
Cardiopulmonary Resuscitation
CPR should be avoided in acute trauma unless there is suspicion of dysrhythmia, pulmonary embolism, or a myocardial infarction prior to the trauma.19 In the absence of a nontraumatic arrest (medical arrest), CPR offers little benefit and may be potentially harmful. Therefore, resuscitative thoracotomy should be considered in traumatic arrests, especially in the setting of penetrating trauma with recent loss of pulses.19 Appropriate precautions should be taken when performing the thoracotomy because it increases the risk of pathogen exposure. Only necessary staff should be immediately present when it is performed. Additionally, it is recommended that early endotracheal intubation be performed prior to CPR to secure the patient’s airway and reduce potential viral transmission to healthcare personnel. Experts call for the use of external chest compression devices when chest compressions are indicated and the use of a bag valve mask with a high-efficiency particulate air filter for the same reason.19
Trauma Surgery Triage
Given the increased shortage of ICU beds because of the pandemic, the heightened risk of COVID-19 exposures in the surgical setting, and the incidence of complications for surgical patients, the threshold for surgery qualification has had to be adjusted.19 Early in the pandemic in countries where elective surgeries and non-urgent clinic visits were permitted to continue as usual, COVID-19 cases increased significantly, as did intrahospital transmission rates and resource utilization.45 Thus, guidelines encouraging the use of nonoperative or conservative management when possible have been developed by healthcare systems globally to reduce both intraoperative surgical times and postoperative hospital stays.45
Surgical prioritization and resource management have been especially challenging for emergency healthcare personnel, since the timing of operative management in such cases is critical. In general, indications for urgent/emergent surgery should not change even in the setting of unprecedented circumstances, such as a pandemic.46 However, factors influenced by the COVID-19 pandemic have compelled emergency healthcare workers to consider alternative options. The following are three fundamental concerns that influence the final therapeutic decision:
• the severity of the traumatic injury and urgency of its intervention;
• the potential of patient and/or healthcare worker infection;
• the impact on hospital infrastructure and resources, including the availability of ICU beds.
The decision to operate or delay surgical intervention while COVID-19 screening results are pending ultimately rests with the treating trauma surgeon.46 The surgeon must take the above three factors into consideration, as well as time-dependent variables, such as mortality and morbidity associated with each individual case.46 A task force of the Chinese Society of Anesthesiology has provided guidance for emergency operative management during the COVID-19 pandemic. These may prove useful when weighing risks and benefits of expedited surgical intervention. They propose the following indications for emergency trauma surgery:19
“(1) Blunt injury with prehospital index (PHI) ≥ 4;
(2) Penetrating injury with hemodynamic instability;
(3) Uncontrolled external hemorrhage;
(4) Traumatic brain injury;
(5) Orthopedic surgeries like fracture fixation, spinal trauma, or decompression;
(6) Any acute care surgery in an admitted COVID-19 patient.”
Indications for urgent surgical intervention also vary among different surgical subspecialties. For instance, oral and maxillofacial trauma specialists (OMFS) have had to establish clarification for urgent operative indications because of the unique risks that accompany working within the oral cavity/nasal-oropharyngeal mucosa of COVID-infected patients because these areas confer a higher risk of transmission because of increased viral particles.21 Moreover, many cases of facial trauma pose significant morbidity and/or mortality to patients without urgent or emergent intervention.22 Even those facial traumas that are not emergent commonly require surgical repair because of potential unfavorable sequelae (e.g., infection and permanent functional or cosmetic deformity) that may be more challenging and require even more resources to treat if delayed.22 As a result, OMFS, plastic surgery, and other reconstructive surgeons have developed a protocol for facial trauma triage during the COVID-19 pandemic.22 Similarly, orthopedic trauma experts have categorized orthopedic injuries along a spectrum of severity and the rapidity with which they require intervention. Trauma teams should coordinate with respective consultants regarding delayed vs. immediate surgical intervention.
Preoperative Recommendations
Several guidelines have been developed for preoperative planning in response to COVID-19 concerns. In general, preoperative management should aim to limit foot traffic and the total number of surgical staff in the OR. It should seek to designate COVID-specific ORs and supply stores to minimize risk to staff, and it should enhance communication among the OR team.47 The designated COVID OR should ideally be a negative pressure environment (alternatively, a relatively isolated room with an independent purification system), allowing for the inflow of air into the OR and outflow of air through a protective filter.48 High frequency air exchange of 25 cycles/hour or more is recommended.48 PPE should be available outside the OR door and donned before entering the OR.48 All necessary equipment should be ready in the OR prior to the start of the case to limit entry and exit throughout the case. OR doors should remain closed during the operation.48
Management of Anesthesia
The choice of anesthetic technique for a trauma patient who is positive or suspected of having SARS-CoV-2 is dependent on several factors, including the patient’s condition, the severity of injury, and the planned procedure.19 In general, regional anesthesia (e.g., neuraxial anesthesia, peripheral nerve block) is the preferred technique because it avoids the potential risk of aerosolization of airway secretions associated with general anesthesia and airway management.19 It is advised that patients not receiving general anesthesia always wear a surgical mask.49 If supplemental oxygen is required, the lowest flows needed to maintain oxygenation should be used.49 In cases when general anesthesia cannot be avoided, such as neurosurgical trauma, thoracoabdominal trauma, and/or polytrauma with shock, endotracheal intubation (as discussed previously in this article) instead of supraglottic devices should be used to effectively seal the airway and prevent viral transmission. Table 2 provides a summary of anesthesia considerations during the COVID-19 pandemic developed by the European Society of Trauma and Emergency Surgery (ESTES).34
Table 2. Anesthesia Considerations During the COVID-19 Pandemic |
|
Adapted from: Coimbra R, Edwards S, Kurihara H, et al. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg 2020;46:508. |
Intraoperative Recommendations
It is recommended that the OR staff not immediately involved with the intubation be outside of the operating theater during and approximately 20-30 minutes following the intubation, if time permits.22 All OR staff should have appropriate PPE (including N95 masks or PAPR), with extra equipment readily available if necessary.34 The operation should be performed preferably by an experienced surgeon. Avoiding the use of such cases for teaching purposes is highly recommended.47 Surgeons should aim to finish an operation within 90 minutes, if possible, to minimize time spent in the OR with potentially high-risk procedures.3 Some strategies have been proposed to shorten operation time, including packing hemostasis, external fixation, and temporary abdominal closure.4 Rinsing and drainage of bodily fluids should be limited to reduce the risk of intraoperative contamination.3 Surgical smoke evacuation is also an important precaution. Many devices (e.g., electrocautery, the ultrasonic harmonic scalpel, and tissue ablation lasers) used in operations produce gaseous microparticles, combustion products, and carbon dioxide, which increase the risk of aerosolizing viral particles.47 Thus, their use should be avoided when possible. Smoke evacuators/filtration devices should be used in cases requiring smoke-producing equipment to limit exposure to aerosols.47
Laparoscopy, a commonly used surgical technique in trauma surgery, is considered a high-risk AGP due to the artificial pneumoperitoneum and smoke generation associated with this technique.31 The laparoscopic approach should be avoided when possible, and the open approach should be prioritized for this reason.31 However, it is important to recognize that laparoscopic approaches are highly effective in decreasing the length of hospital stays. Therefore, experts recommend that surgeons weigh the advantages and disadvantages of the intended surgical approach on a case-by-case basis.31
Postoperative Recommendations
For patients who are extubated after their operation, full recovery in the OR for up to 60 minutes is advised prior to transport.47 Otherwise, a dedicated COVID-19 transport ventilator should be used if a patient is to remain intubated post-surgical intervention.47 Suspected or confirmed COVID-19 trauma patients should be transported to an isolated hospital room until their PCR results return.3 If possible, postoperative documentation should be completed outside of the OR.34
The PPE used by OR staff must be properly removed and disposed of, and proper hand washing should immediately follow the doffing of PPE.25,34,47 (See Figure 3, available online: https://bit.ly/3g9IQxv.) The surgical team should change into new surgical scrubs after the end of the case.34 Meticulous cleaning of the OR is crucial following surgical cases. Previous reports have noted that human coronaviruses can remain on uncleaned surfaces for days, but they may be eliminated with disinfectants that consist of 70% ethanol, 0.1% sodium hypochlorite, or 0.5% hydrogen peroxide.47 Hospital staff involved in the cleaning process should be well-trained and wear full PPE, similar to that worn by OR staff throughout operations.47
It is important to monitor trauma patients closely for signs and symptoms of COVID-19 postoperatively, since this cohort of patients may have impairments in immune function both post trauma and surgical intervention.19 Thus, noninfected trauma patients may have a higher risk of nosocomial infection in the perioperative/postoperative setting. Healthcare personnel should be proactive in screening and treating for postoperative thrombosis such as deep vein thrombosis/pulmonary embolism, especially in SARS-CoV-2-positive patients, since there appears to be an increased association between COVID-19 and thrombosis.19 Given this, prompt prophylactic anticoagulation with low molecular weight heparin (LMWH) in suspected or confirmed COVID-positive surgical patients is recommended.31
Future Considerations
The recent lifting of shelter-in-place restrictions as well as the development of COVID-19 vaccines potentially may have helped diminish some of the unique obstacles faced by healthcare workers since the start of the pandemic. However, significant challenges have arisen in the post-lockdown phase, necessitating that emergency/trauma providers remain vigilant and flexible. Specifically, the easing of public restrictions has been accompanied by an emergence of new SARS-CoV-2 variants and surges of COVID-19 cases.50-52 Moreover, hospital inpatient censuses have increased along with the number of trauma patients.19 It is evident that the demand for healthcare resources will continue to rise. Therefore, frequent updates to best practice guidelines detailing improvements and advancements to trauma care in the face of a persistent pandemic remain a vital necessity.
Summary
Both SARS-CoV-2 and the accompanying public lockdown measures affected healthcare systems tremendously, overwhelming hospitals with increasing demand for already strained resources. Additionally, the public fear of potential viral transmission and government mandated stay-at-home orders altered the frequency, severity, and presentations of traumatic injuries.
In response, emergency healthcare systems had to modify various aspects of trauma care. Guidelines have been developed for the types of PPE personnel must wear and for the systematic organization of the trauma bay to minimize the risk of viral spread. Additionally, procedures for COVID-19 screening have been established with recommendations to treat trauma patients as COVID-positive cases in urgent/emergent situations when screening is not feasible. Given the limitations associated with the increased use of PPE, a greater emphasis has been placed on imaging modalities for injury assessment.
New strategies for airway management and resuscitation, including those for intubation, cricothyrotomy, thoracostomy, and CPR, that attempt to limit aerosol generation when possible have been developed as well. Experts also have presented recommendations for triage and disposition in the era of COVID-19. When surgery is deemed necessary, regional anesthesia is preferred over general anesthesia. Open approaches are recommended over laparoscopic approaches when feasible, and additional barriers and time constraints have been offered. Finally, several strategies to minimize viral transmission to healthcare workers and patients during surgical interventions have been proposed. As healthcare systems continue to care for patients in the face of evolving research, emerging COVID-19 variants, and increased COVID cases, it will be important to continuously update how to best deliver trauma centered care.
REFERENCES
- Dumovich J, Singh P. Physiology, trauma. In: StatPearls [Internet]. StatPearls Publishing; 2021.
- Parasher A. COVID-19: Current understanding of its pathophysiology, clinical presentation, and treatment. Postgrad Med J 2021;97:312-320.
- Li Y, Zeng L, Li Z, et al. Emergency trauma care during the outbreak of corona virus disease 2019 (COVID-19) in China. World J Emerg Surg 2020;15:33.
- Halaji M, Heiat M, Faraji N, Ranjbar R. Epidemiology of COVID-19: An updated review. J Res Med Sci 2021;26:82.
- Bohn MK, Hall A, Sepiashvili L, et al. Pathophysiology of COVID-19: Mechanisms underlying disease severity and progression. Physiology (Bethesda) 2020;35:288-301.
- Bessoff KE, Han RW, Cho M, et al. Epidemiology of pediatric trauma during the COVID-19 pandemic shelter in place. Surg Open Sci 2021;6:5-9.
- Jeffery MM, D’Onofrio G, Paek H, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med 2020;180:1328-1333.
- Waseem S, Nayar SK, Hull P, et al. The global burden of trauma during the COVID-19 pandemic: A scoping review. J Clin Orthop Trauma 2021;12:200-207.
- Ferron R, Agarwal G, Cooper R, Munkley D. The effect of COVID-19 on emergency medical service call volumes and patient acuity: A cross-sectional study in Niagara, Ontario. BMC Emerg Med 2021;21:39.
- Rosenbaum J, Lucas N, Zandrow G, et al. Impact of a shelter-in-place order during the COVID-19 pandemic on the incidence of opioid overdoses. Am J Emerg Med 2021;41:51.
- DiFazio LT, Curran T, Bilaniuk JW, et al. The impact of the COVID-19 pandemic on hospital admissions for trauma and acute care surgery. Am Surg 2020;86:901-903.
- Butt AA, Azad AM, Kartha AB, et al. Volume and acuity of emergency department visits prior to and after COVID-19. J Emerg Med 2020;59:730-734.
- Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699-704.
- Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA 2020;324:96-99.
- Jacob S, Mwagiru D, Thakur I, et al. Impact of societal restrictions and lockdown on trauma admissions during the COVID-19 pandemic: A single-centre cross-sectional observational study. ANZ J Surg 2020;90:2227-2231.
- Rajput K, Sud A, Rees M, Rutka O. Epidemiology of trauma presentations to a major trauma centre in the North West of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg 2021;47:631-636.
- McGraw C, Salottolo K, Carrick M, et al. Patterns of alcohol and drug utilization in trauma patients during the COVID-19 pandemic at six trauma centers. Inj Epidemiol 2021;8:1-8.
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061-1069.
- Sawhney C, Singh Y, Jain K, et al. Trauma care and COVID-19 pandemic. Anaesthesiol Clin Pharmacol 2020;36:1-6.
- Haut ER, Leeds IL, Livingston DH. The effect on trauma care secondary to the COVID-19 pandemic: Collateral damage from diversion of resources. Ann Surg 2020;272:e204.
- Holmes S, Bhatti N, Bhandari R, Chatzopoulou D. Toward a consensus view in the management of acute facial injuries during the Covid-19 pandemic. Br J Oral Maxillofac Surg 2020;58:571-576.
- Hsieh TY, Dedhia RD, Chiao W, et al. A guide to facial trauma triage and precautions in the COVID-19 pandemic. Facial Plast Surg Aesthet Med 2020;22:164-169.
- Douedi S, Douedi H. Precautions, bloodborne, contact, and droplet. In: StatPearls [Internet]. StatPearls Publishing; 2021.
- Schmitz D, Vos M, Stolmeijer R, et al. Association between personal protective equipment and SARS-CoV-2 infection risk in emergency department healthcare workers. Eur J Emerg Med 2021;28:202-209.
- The National Institute for Occupational Safety and Health (NIOSH). COVID-19 Personal Protective Equipment (PPE). Centers for Disease Control and Prevention. Page last reviewed Oct. 5, 2021. https://www.cdc.gov/niosh/emres/2019_ncov_ppe.html
- Livingston DH, Bonne S, Morello C, Fox A. Optimizing the trauma resuscitation bay during the Covid-19 pandemic. Trauma Surg Acute Care Open 2020;5:e000488.
- Centers for Disease Control and Prevention. COVID-19. First responders. Updated July 15, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-for-ems.html
- Goodloe JM, Topjian A, Hsu A, et al. Interim guidance for emergency medical services management of out-of-hospital cardiac arrest during the COVID-19 pandemic. Circ Cardiovasc Qual Outcomes 2021;14:e007666.
- Gök AFK, Eryllmaz M, Ozmen MM, et al. Recommendations for trauma and emergency general surgery practice during COVID-19 pandemic. Ulus Travma Acil Cerrahi Derg 2020;26:335-342.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth 2020;67:568-576.
- De Simone B, Chouillard E, Sartelli M, et al. The management of surgical patients in the emergency setting during COVID-19 pandemic: The WSES position paper. World J Emerg Surg 2021;16:14.
- Gonzalez JM, Crenshaw N, Larrieu-Jimenez P, et al. Point-of-care lung ultrasonography: A clinical update for the emergency nurse practitioner. Adv Emerg Nurs J 2021;43:279-292.
- Tung-Chen Y, Algora-Martín A, Llamas-Fuentes R, et al. Point-of-care ultrasonography in the initial characterization of patients with COVID-19. Med Clin (Barc) 2021;156:477.
- Coimbra R, Edwards S, Kurihara H, et al. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg 2020;46:505-510.
- Cook TM, El-Boghdadly K, McGuire B, et al. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the intensive care society, the faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020;75:785.
- Luo M, Cao S, Wei L, et al. Precautions for intubating patients with COVID-19. Anesthesiology 2020;132:1616-1618.
- Shrimpton AJ, Brown JM, Gregson FKA, et al. Quantitative evaluation of aerosol generation during manual facemask ventilation. Anaesthesia 2022;77:22.
- Meng L, Oiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology 2020;132:1317-1332.
- Orser BA. Recommendations for endotracheal intubation of COVID-19 patients. Anesth Analg 2020;130:1109.
- Chen X, Liu Y, Gong Y, et al. Perioperative management of patients infected with the novel coronavirus: Recommendation from the joint task force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology 2020;132:1307-1316.
- Gottlieb M, Alerhand S, Long B. Point-of-care ultrasound for intubation confirmation of COVID-19 patients. West J Emerg Med 2020;21:1042.
- Canelli R, Connor CW, Gonzalez M, et al. Barrier enclosure during endotracheal intubation. N Engl J Med 2020;382:1957-1958.
- Issa N, Liddy WE, Samant S, et al. Emergency cricothyrotomy during the COVID-19 pandemic: How to suppress aerosolization. Trauma Surg Acute Care Open 2020;5:e000542.
- Pieracci FM, Burlew CC, Spain D, et al. Tube thoracostomy during the COVID-19 pandemic: Guidance and recommendations from the AAST Acute Care Surgery and Critical Care Committees. Trauma Surg Acute Care Open 2020;5:498.
- Brindle ME, Doherty G, Lillemoe K, Gawande A. Approaching surgical triage during the COVID-19 pandemic. Ann Surg 2020;272:e40.
- Aranda-Narváez JM, Tallón-Aguilar L, Pareja-Ciuró, et al. [Emergency surgery and trauma care during COVID-19 pandemic. Recommendations of the Spanish Association of Surgeons]. Cir Esp (Engl Ed) 2020;98:433.
- Heffernan DS, Evans HL, Huston JM, et al. Surgical Infection Society guidance for operative and peri-operative care of adult patients infected by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Surg Infect 2020;21:301-308.
- Tan Chor Lip H, Huei TJ, Mohamad Y, et al. Critical adjustments and trauma surgery trends in adaptation to COVID-19 pandemic in Malaysia. Chin J Traumatol 2020;23:207.
- Uppal V, Sondekoppam RV, Landau R, et al. Neuraxial anaesthesia and peripheral nerve blocks during the COVID-19 pandemic: A literature review and practice recommendations. Anesthesia 2020;75:1350-1363.
- Hussein NR, Naquid IA, Saleem ZSM, et al. A sharp increase in the number of COVID-19 cases and case fatality rates after lifting the lockdown in Kurdistan region of Iraq. Ann Med Surg 2020;57:140-142.
- Brown CM, Vostok J, Johnson H, et al. Outbreak of SARS-CoV-2 infections, including COVID-19 vaccine breakthrough infections, associated with large public gatherings—Barnstable County, Massachusetts, July 2021. MMWR Morb Mortal Wkly Rep 2021;70:1059-1062.
- Chia PY, Ong SWX, Chiew CJ, et al. Virological and serological kinetics of SARS-CoV-2 delta variant vaccine breakthrough infections: A multicentre cohort study. Clin Microbiol Infect 2021; Nov 23. doi: 10.1016/j.cmi.2021.11.010. [Online ahead of print].
COVID-19 has affected every aspect of medical care. The authors discuss modifications of trauma care to protect both patients and providers.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.