Fighting and Beating Sepsis Mortality Rates
January 1, 2016
Reprints
Executive Summary
Two different hospital systems have made sizable dents in their sepsis mortality rates through a collaborative process between emergency and ICU staff. At Northwest Hospital in Randallstown, MD, success occurred, in part, by lowering the threshold for transfer of emergency patients with signs of sepsis to the ICU. Voorhees, NJ-based Kennedy Health has lowered sepsis mortality rates by taking steps to integrate the care of sepsis patients between the ED and the ICU, and slashing the time required to deliver bundle-oriented care.
- Research conducted at Northwest Hospital shows that sepsis mortality decreased by nearly half, going from 14.38% before intervention to 7.85% following implementation of the lower ICU thresholds.
- Clinical leaders at Kennedy Health report that they have lowered sepsis mortality from the mid-20% range to less than 12% through a collaborative approach involving all stakeholders.
- Sources from both hospitals stress the importance of using data to achieve buy-in to improvement efforts, and giving interventions enough time to take hold.
At first glance, it seems counterintuitive that lowering the thresholds required for ED patients with sepsis to be transferred to ICUs would actually boost the efficient use of precious ICU resources. However, a new study conducted at Northwest Hospital in Randallstown, MD, shows that not only can just such a change improve utilization of the ICU, it can also substantially improve sepsis outcomes.
Comparing sepsis mortality before and after implementation of the policy change, investigators reported that sepsis mortality decreased by more than 45% after lowering sepsis thresholds, reducing sepsis mortality from 14.38% to 7.85%, even though there was no change in illness severity. Further, the ICU length of stay (LOS) was 25.9% lower in patients observed following implementation of the lower thresholds. The retrospective study involved the review of a total of 886 medical records from patients who were diagnosed with sepsis.1
The findings, which were first reported at the annual meeting of the American College of Chest Physicians held in Montreal in late October, are only in abstract form at this point, but researchers report that the results have since been largely replicated at Sinai Hospital in Baltimore, a much larger hospital with a 29-bed ICU. Both Northwest Hospital and Sinai Hospital are part of LifeBridge Health, so many clinicians serve both facilities.
However, the researchers suggested that a lynchpin for achieving success with this tactic is developing a collaborative culture between the ED and the ICU. It is a sentiment that is shared by clinical leaders at Kennedy Health, an organization which has also substantially driven down sepsis mortality rates at its three acute care hospitals through a similar process.
Joseph Carrington, DO, MHA, a co-author of the Northwest Hospital study and a third year internal medicine resident at Sinai Hospital, explains that what prompted the change at Northwest was the data around sepsis and ICU utilization.
“We looked at our numbers and recognized that we had a lot of patients in our ICU who were there for more than seven days, and sometimes more than 14 days, which was obviously clogging our ICU,” he says.
In addition, Carrington notes that the mortality rates for sepsis were higher than the national average.
“We really didn’t know why these things were happening, but we decided to get together,” Carrington observes. “We formed a group with the emergency physicians and the ICU physicians and talked openly about what was going on, and we performed sort of a root cause analysis of [the problems].”
What the group discovered was that many patients who presented to the ED were considered borderline for sepsis, and they would either end up sitting in the ED for long periods of time while clinicians tried three or more interventions, or they would be admitted to the hospital’s intermediate care service to receive the interventions.
“But they didn’t have somebody really taking ownership over them and giving them all the support they needed early on, so they did worse,” Carrington says. “They had higher mortality. They needed transfers to our ICU. By the time we got them [in the ICU] they were so sick that they ended up staying there for a week or longer, sometimes requiring [tracheotomies] and everything else.”
The group working through this problem came to realize that the emergency physicians themselves perceived that there were barriers preventing them from sending patients to the ICU earlier, Carrington explains. For instance, an emergency physician might feel like he needed to at least attempt to treat the borderline sepsis patients, either because, in his mind, it would mean he is a better physician or because the ICU has a limited number of beds, which are reserved for the sickest patients.
To address the issue, ICU physicians and emergency physicians decided to set parameters on when a patient should be sent to the ICU.
“If somebody was in true septic shock with a lactate of four, then we sent them no matter what, even if they looked OK,” Carrington explains. “Let’s just invest in them earlier and get them to the ICU.”
When treating a borderline sepsis patient in the ED, the group decided that if a first intervention fails, the patient should then be sent to the ICU.
“We disseminated this change throughout the ED and the ICU,” Carrington says, noting that physicians were informed that patients would be accepted into the ICU, no questions asked. “It was really a process of getting everybody together to think about what was going wrong and how we could change it.”
Be transparent
Carrington acknowledges that one of the group’s biggest fears was that the 16-bed ICU at Northwest would be overrun with patients as a result of this change.
“We were already running at a pretty high capacity,” he says. Sure enough, for the first couple of months, there were a lot of extra patients arriving at the ICU, and the unit needed to borrow beds from other areas to deal with the demand, Carrington says. “Also, there were certainly some people doubting the process,” he says. “They would look at the patients, say they are not intubated, and ask what they are doing [in the ICU].”
However, after those first couple of months, demand on the ICU eased and stabilized.
“The long LOS patients decreased enough that our daily census returned to what we were seeing before,” Carrington observes. “Most of the patients coming into the ICU are only staying three days instead of longer, and then going out and making room for the next batch of patients.”
Carrington does allow that most of the early pushback came from ICU clinicians. The emergency physicians largely embraced the concept.
“[Emergency physicians] loved the idea of having an intensivist come down to the ED, lay their eyes on the patient, make sure the orders are there, and make sure that everything is correct … especially for septic patients that needed an intervention early on,” he says.
Carrington adds that placing those patients in an ICU sooner rather than later makes the job easier for emergency physicians, but it is also better for the sepsis patients to have dedicated nursing staff with them.
With substantial reductions in mortality, there is no doubt that the approach has been successful, at least at the LifeBridge hospitals. For other organizations interested in following a similar path, Carrington advises that the best way to achieve buy-in during the early days is to be transparent and to fully leverage your data.
“The most successful thing was sitting down and putting the mortality figures in front of people,” Carrington notes. “For the people who were doubting the system and feeling a little overworked at the beginning in the ICU … we simply came to them and said, ‘here are our mortality rates for sepsis and here is the national average.’ That kind of shocked people because it wasn’t something that was openly talked about with the people who are on the frontlines delivering care. It is usually something that is reported behind doors to administrators and board members.”
That’s when the people who are actually delivering the care realized they could do better, Carrington says. “Suddenly, they started stepping up and saying, ‘What can I do? How can I make this transition happen?’” he says. “That was the most important thing.”
Begin with awareness, education
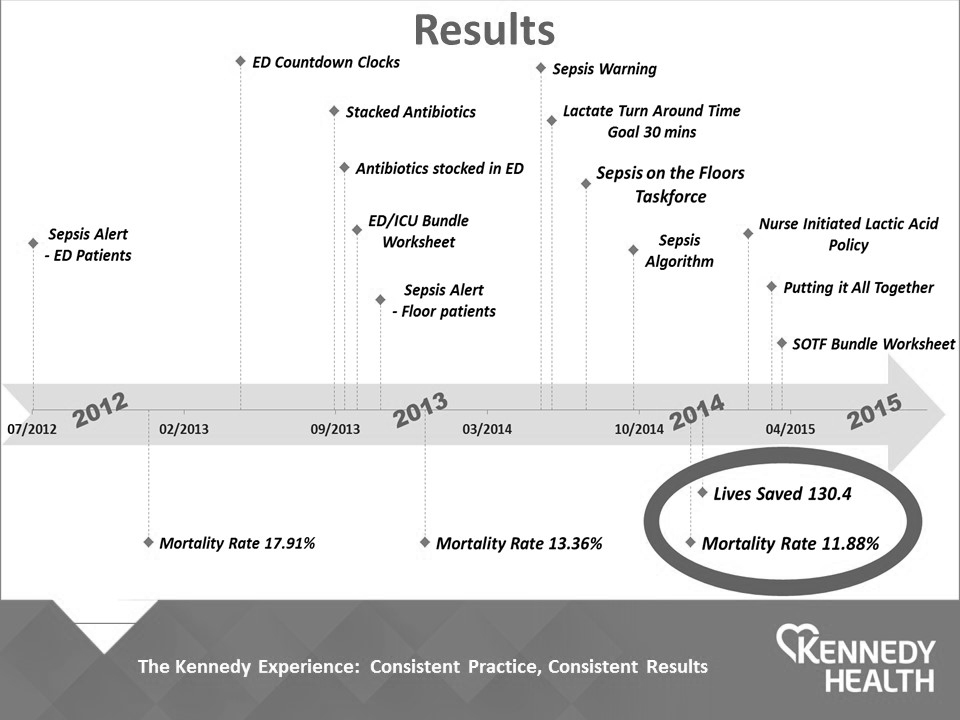
With sepsis mortality rates in the mid-20% range, Kennedy Health began focusing intently on sepsis in 2012. Henry Schuitema, DO, the system section head of emergency medicine and medical director of the ED at the Stratford, NJ, campus of Kennedy University Hospital, and Marianne Kraemer, RN, EdM, MPA, CCRN, the chief nursing officer at both Kennedy Health and the Stratford campus, co-chaired a new sepsis committee that drove the process.
“The vast majority of our patients are admitted through the [health system’s three] EDs, so our decision was to [initially] focus on the EDs in identifying sepsis and then work collaboratively with the ICUs so that we could move patients quickly once they were identified … and really get rolling on knocking down some of those important bundle elements,” Schuitema explains. “We started with what was a called a sepsis alert, and that was a patient who came into the ED who was either hypotensive despite aggressive fluid resuscitation or they had a lactate greater than four.”
When the ED identified a patient meeting these criteria, a sepsis alert would sound overhead, and a nursing supervisor would identify a bed in the ICU, an ICU nurse manager would ensure that a bed was available, and an intensivist and the ICU team would respond immediately to the ED to see what they could do to bring the patient to the unit, Schuitema says.
“We started that in 2012, and by February 2013 our sepsis mortality rate had dropped to 17.91%,” he adds.
With further improvements, the sepsis mortality figure has dipped to below 12%, but both Schuitema and Kraemer stress that the effort requires a strong and continuous focus. (See the figure below.)
Kraemer notes that key to the early success of the approach was an educational effort aimed at equipping the emergency nurses with the knowledge and skill to recognize the early signs of sepsis, and what to do after a sepsis diagnosis. It was also essential to quickly gather all the lab work required in the sepsis bundle.
“Initially it was a six-hour bundle and now it is down to a three-hour bundle,” Kraemer explains. “Through the creativity of the ED nursing staff and nursing leadership, they ended up buying a countdown clock that they would set, and it would count down so that they would be constantly reminded how close they were to zero, when [all of the bundle elements] had to be done.”
ED nursing has critical role
Nursing leadership from all three hospitals in the Kennedy Health organization worked closely with emergency physicians to drive the improvement process, Schuitema observes.
“We have a performance review committee that looks not only at throughput, but also a lot of our quality measures, and out of that committee grew educational endeavors,” he says. “We taught the residents from emergency medicine, and the nurse educators were very aggressive at educating the heck out of the nurses, to the point where the ED nurses are now very astute at recognizing sepsis.”
In fact, Schuitema notes that the nurses are now calling out sepsis warnings from triage.
“If a patient arrives and they have SIRS [systemic inflammatory response syndrome] criteria at triage, they will call a sepsis warning very much like they would call a stroke alert or a code STEMI [ST-segment elevation myocardial infarction] for an MI,” he says. “These patients will come right from triage with a temperature of 103 and SIRS criteria, and within 15 minutes of arrival they will have volume resuscitation already initiated and antibiotics planned. [Nursing leaders] were incredibly important in driving this.”
Some other process improvement initiatives that were underway at Kennedy Health also contributed to the sepsis effort, Kraemer adds.
“The EDs had a higher than average blood culture contamination rate, so the ED educators were looking at that and working with staff to get that parameter back way under baseline,” she says. “They were doing very well with it, and that little process improvement initiative kind of spilled over into everything else they were doing with sepsis.”
The nurses used the same model of looking at a process that was broken, and then fixing it piece by piece, Kraemer notes. “They were putting all these little pieces together and making this major process improvement performance initiative really go very well,” she says.
Integrate pharmacy
Pharmacy also played a role in the improvement initiative, Schuitema says. For instance, when the sepsis initiative began, all the antibiotics were stocked in the hospital pharmacy, so when an emergency physician prescribed antibiotics for a sepsis patient, the pharmacy would bring the antibiotics to the department. However, the sepsis committee observed that this was costing valuable time.
“Fifteen minutes doesn’t seem like a lot of time, but we realized that we really needed to keep these antibiotics stocked in the ED,” Schuitema explains.
Further, as a result of literature searches, Schuitema notes that clinicians realized that the research didn’t necessarily support running just one antibiotic at a time in the sickest patients, so clinicians began prescribing two antibiotics at a time.
“That, too, was a hurdle, but the ED team did a very good job of working through it,” he says.
Also, to more tightly integrate the care of sepsis patients in the ED and the ICU, nursing from the two departments created an ED/ICU bundle worksheet that goes into effect as soon as a patient arrives in the ED.
“Once complete, the ED piece goes to the ICU,” Schuitema notes. “The ICU then takes ownership of that worksheet.”
By documenting all the care that patients receive as well as the timing of this care, clinicians have been successful at accelerating the treatment path.
“We were able to very easily collect the amount of volume the patient was receiving in the ED, the time of the antibiotics, and we have been very successful at getting our antibiotics in within not only a three-hour bundle, but now we have a reach goal of trying to get [the antibiotics] in within a one-hour bundle,” Schuitema says.
Eliminate time wasters
Of course, it is not easy to identify all patients as septic early on, Schuitema acknowledges.
“We had a patient who was in here yesterday who had a headache and was vomiting. Her vital signs were normal in triage with the exception of a heart rate of 120, but she wasn’t febrile,” he explains. “Over the course of her evaluation [her temperature] spiked to 102. Suddenly, fears shifted. Lactates were sent, and it turns out the patient was indeed septic.”
In that case, the patient received antibiotics four hours after her arrival to the ED, although they were administered within two hours of the identification of sepsis.
“We try to perfect the system as best we can, recognizing that not everyone comes in with a stamp across their forehead saying they are septic,” Schuitema observes. “You get patients who are very difficult to figure out.”
While a diagnosis of sepsis may take longer in some patients, the data-driven improvement process has enabled clinicians to focus in on processes that were taking too long to complete. For example, Kraemer notes that when it became clear that waiting for results from lactate tests put a drag on care, the sepsis committee focused on every step, from ordering a test to results arriving in the ED, to determine the delay.
“When we actually looked at all the individual elements, we could see areas that were time wasters … so we streamlined the process,” Kraemer explains. “Also, as a result of that work, we were able to pass through our medical executive board a nurse-initiated lactic acid policy where, based on two SIRS criteria, a nurse can draw lactic acid independent of a physician order. That was a big deal.”
Involve the right stakeholders
Despite the implementation of a number of process changes, there has been very little pushback, Schuitema observes, and he suspects the reason why is because the right people were at the table from the beginning.
“When this [sepsis] committee formed, we put it together with physicians who were all players and had skin in the game … so we have several emergency physicians from each of our campuses. We have the ICU/intensivist team. We have the hospitalist team that manages folks on the floors as well as the units. We also have our IT people,” he explains, adding that representatives from pharmacy, respiratory, nursing, and senior leadership are also involved.
“There were a couple of physicians who never play well in the sandbox and continue to not play well, but we were able to redirect them by showing them their fallouts and showing them their cases. They came into compliance kicking and screaming, but that was an isolated issue that isn’t unique to any medical staff,” Schuitema says.
In fact, central to the success of the initiative is ongoing and rigorous performance review.
“We have a group of nurses, and their job is to review charts on core measures and quality issues. They do it in real time,” Schuitema explains. “If there is a patient who … is up in the ICU with a diagnosis of sepsis, they are on that at 8 a.m., and they are reviewing the chart to see if the patient satisfied the bundle elements.”
Schuitema notes that he will receive an email quickly if the clinical team has fallen short of expectations.
“I will review the chart, and usually within 24 hours I am able to give feedback to those players that were involved,” he explains.
With such close and constant review, the sepsis committee was able to pick up on the fact that sepsis performance has a tendency to suffer when new residents arrive, so committee members took steps to enhance education of new residents to ensure they have a better understanding of both the sepsis bundle timelines and the workflow of the ED, Schuitema says.
The sepsis committee, which meets every other month, reviews any instances in which performance does not meet expectations.
“When there are fallouts we talk about it in committee and look at it from a lessons learned standpoint,” Kraemer notes. “We drill down. What part of the bundle did we not do well or time well? That is how we review the cases.”
Set the right tone
It has taken time to address such issues in a non-punitive fashion, but Kraemer observes that the hospital system has been working toward instituting such a culture in parallel with the sepsis improvement efforts.
“I am also the administrator overseeing the infection control program within all three hospitals … and whenever we have a device-related infection, a central line infection, or a catheter-associated UTI [urinary tract infection] … we pull the team together, review the case, look at it as a lesson learned … and make sure other hospitals [in the Kennedy system] receive the information,” she explains. “We don’t accuse someone of wrongdoing. We look at it so that we don’t do it again.”
Kraemer advises colleagues who are interested in improving their performance on sepsis to be prepared for setbacks, but remain persistent.
“In our first few years of collecting data, we couldn’t see a story from it. We couldn’t see quite where it was going. But we stuck with it and then suddenly one thing was working,” she says. “You take two steps forward and one step back, but you stay with it and keep looking at whether the data tells a story. You have to wait until you can see it.”
REFERENCE
- Carrington J, Barnes J. Making ICU admissions smarter, not making them harder: Lowering ICU admission thresholds improves outcomes and resource utilization. Chest 2015;148 (4_Meeting Abstracts):246A. doi:10.1378/chest.2270816.
SOURCES
- Joseph Carrington, DO, MHA, Resident, Internal Medicine, Sinai Hospital, Baltimore. Phone: (410) 601-9000.
- Marianne Kraemer, RN, EdM, MPA, CCRN, Chief Nursing Officer, Kennedy Health, Voorhees, NJ, and Chief Nursing Officer, Kennedy University Hospital, Stratford, NJ. E-mail: [email protected].
- Henry Schuitema, DO, System Section Head, Emergency Medicine, Kennedy Health, Voorhees, NJ, and Medical Director, Emergency Department, Kennedy University Hospital, Stratford, NJ. E-mail: [email protected].
Lower ICU thresholds, earlier identification, and decreased times-to-treatment are fueling better outcomes.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
