Pediatric Visceral Trauma
August 1, 2016
Reprints
AUTHORS
Molly Wormley, MD, Chief Resident, University of Arizona, Tucson.
Aaron Leetch, MD, Assistant Professor, Departments of Emergency Medicine and Pediatrics; Associate Program Director, Emergency Medicine/Pediatrics Residency, University of Arizona, Tucson.
PEER REVIEWER
Taryn Taylor, MD, FAAP, FACEP, Assistant Professor of Pediatrics and Emergency Medicine, Emory University School of Medicine, Atlanta, GA.
To reveal any potential bias in this publication, and in accordance with Accreditation Council for Continuing Medical Education guidelines, we disclose that Dr. Farel (CME question reviewer) owns stock in Johnson & Johnson. Dr. Stapczynski (editor) owns stock in Pfizer, Johnson & Johnson, Walgreens Boots Alliance Inc., GlaxoSmithKline, Bristol Myers Squibb, and AxoGen. Dr. Schneider (editor), Ms. Fessler (nurse planner), Dr. Wormley (author), Dr. Leetch (author), Dr. Taylor (peer reviewer), Ms. Mark (executive editor), Ms. Coplin (executive editor), and Mr. Landenberger (editorial and continuing education director) report no financial relationships with companies related to the field of study covered by this CME activity.
EXECUTIVE SUMMARY
- Trauma is the leading cause of death in children older than 1 year. Blunt trauma is more common than penetrating trauma.
- A lap belt sign or seat belt sign is a hematoma on the abdomen after a motor vehicle crash. It is associated with hollow viscus injuries as well as other intra-abdominal injuries and Chance fractures of the lumbar spine.
- Intra-abdominal injury correlates with an elevated AST, decreased hematocrit, and abnormal abdominal exam and an abnormal chest X-ray. Hematuria is also a significant finding.
- A FAST exam is often used to assess for intra-abdominal injury. A CT scan may be necessary if there is an equivocal exam or the patient becomes hemodynamically impaired.
Trauma patients are often very difficult to assess, particularly young children. Young people have significant cardiovascular reserve. They will maintain their blood pressure and pulse in the normal range while their body is hemorrhaging. Most of us have experienced the sudden crash of a “stable” patient. This article reviews trauma in children. It reminds us that children are not little adults. Their injury pattern and their response to injury are unique.
— The Editor
Etiology
Trauma is a leading cause of morbidity and mortality in children older than 1 year of age.1 Blunt trauma accounts for about 90% of all pediatric injuries. Falls and motor vehicle collisions represent the most common mechanisms of injury. Head and extremity injuries happen most frequently; however, injury to the abdomen can occur in up to 8% of children and is responsible for 9% of all pediatric trauma deaths.2 (See Table 1.) Thoracic trauma in particular is associated with multisystem trauma and a high risk of mortality. The prevalence of non-accidental trauma and accidental firearm injuries is rising in all populations but is particularly serious in children.
Specific injury patterns to consider include:
- Bicycle handlebar injury: liver, spleen, or pancreatic injury (can be isolated);
- Lap-belt injury: abdominal wall contusion/abrasion/hematoma, small bowel contusion or bowel/organ rupture, distraction fracture of thoracolumbar spine (Chance fracture), traumatic hernia, vascular injury;
- Shoulder harness: bowel/organ injury, traumatic hernia, vascular injury;
- Suspected non-accidental trauma: hollow viscus injury or pancreatic laceration in the setting of retinal hemorrhages, intracranial hemorrhage, or skull, rib, or long bone fractures.
Table 1. Types of Visceral Trauma
Chest
- Pneumothorax ± tension
- Hemothorax
- Pulmonary contusion
- Rib fractures
- Mediastinal injury (less common)
- Diaphragmatic rupture (rare)
- Aortic transection (rare)
- Tracheobronchial tear (rare)
- Flail chest (rare)
- Cardiac contusion/tamponade (rare)
- Esophageal rupture (rare)
Abdomen
- Splenic injury (most common)
- Hepatic injury
- Pancreatic injury
- Bowel hematoma (duodenum)
- Small bowel perforation (jejunum)
- Hollow viscus rupture
- Mesenteric injury
Pelvis/Genitourinary
- Urethral injury
- Bladder rupture
- Renal injury
Chest Trauma
Pliable ribs, diaphragm dependence, and a relatively mobile mediastinum distinguish pediatric chest trauma from adult trauma. Children are less likely to sustain rib fractures, but pulmonary contusions may occur with minimal external signs of trauma. Children with infiltrates on chest radiograph or persistent increased work of breathing likely have sustained pulmonary contusions.3 Pulmonary contusions may take hours to fully manifest, both clinically and radiographically, and these children are at high risk for developing worsening respiratory distress and failure. (See Table 2.) Children who have rib fractures visible on chest X-ray often have underlying contusions as well. Two or more fractures of sequential ribs may result in a flail chest, which negates the typical effort of normal negative pressure breathing and frequently leads to respiratory failure. These children may benefit from early intubation and mechanical ventilation.
Table 2. Thoracic Injuries
Thoracic Injury |
Recognition |
Management |
|
Pneumothorax |
• Difficulty breathing • Chest pain • Decreased breath sounds |
Simple (non-expanding, < 20%): • High-flow oxygen • Chest X-ray > 20% • Needle aspiration • Tube thoracostomy Tension • Emergent needle decompression or tube thoracostomy |
|
Hemothorax |
• Difficulty breathing • Chest pain • Decreased breath sounds |
Simple • Chest X-ray • Tube thoracostomy Massive • Tube thoracostomy • OR thoracotomy – Indications for operative thoracotomy: immediate
chest tube drainage > 10-15 mL/kg or exceeding |
|
Pulmonary Contusion |
• Difficulty breathing • Hypoxia |
• High-flow oxygen • Chest X-ray • Positive pressure ventilation/intubation |
|
Tracheobronchial Rupture |
• Difficulty breathing • Hemoptysis • Subcutaneous emphysema • Persistent pneumothorax despite chest tube decompression |
• CT chest or bronchoscopy if stable • OR thoracotomy • Delayed operative repair |
|
Sucking Chest Wound |
• Bubbling or obvious air escape from chest wound |
• Three-sided occlusive dressing (initially) • Chest tube placement and definitive closure of wound |
|
Blunt Cardiac Injury |
• Chest pain • Sternal fracture • Poor perfusion • Dysrhythmias • Muffled heart sounds (in pericardial tamponade) |
• ECG • Continuous cardiac monitoring • Pericardiocentesis/pericardial window for tamponade |
|
Aortic Rupture |
• Shock/poor perfusion • Chest X-ray findings – Wide mediastinum – Hazy aortic knob – Wide paratracheal stripe – Apical cap – Left hemothorax – First rib fracture |
• CT chest if stable • OR thoracotomy |
|
Mediastinal Penetration |
• Penetrating trauma to any part of the chest • Hemoptysis • Hematemesis |
• Chest X-ray • CT chest/angiography if stable • Tube thoracostomy • OR thoracotomy • Bronchoscopy • Esophagoscopy |
|
Diaphragmatic Injury |
• Difficulty breathing • Poor chest excursion • NG tube deviation on chest X-ray |
• Chest X-ray • CT scan if stable • Exploratory laparoscopy |
|
Traumatic Asphyxia |
• Plethora • Petechiae above injury |
• Evaluate for other injury related to crush • Evaluate for cerebral edema |
Blunt and penetrating chest trauma may result in the development of a pneumothorax. A simple pneumothorax may be asymptomatic or associated with chest pain, respiratory distress, or respiratory failure. On auscultation of the lungs, decreased breath sounds on the affected side may be appreciated. A chest X-ray confirms the diagnosis. Small (< 20%) and asymptomatic or minimally symptomatic pneumothoraces may be treated safely with 100% oxygen and observation for a minimum of four to six hours.4 If a repeat chest X-ray shows improvement, the patient may be discharged home with close follow-up. Larger pneumothoraces benefit from active decompression via tube thoracostomy. Positive pressure ventilation may cause a pneumothorax to enlarge, but small occult pneumothorax diagnosed only on CT may be observed in a stable patient regardless of positive pressure ventilation.
Hemothoraces are best treated with tube thoracostomy. The most common site of chest tube placement is the mid- or anterior axillary line in the fourth intercostal space. The tube should be directed posteriorly and cephalad. The rate of output is used to determine the need for operative thoracotomy. It is best to consult a surgeon if a significant hemothorax is found. The hemodynamic status of the patient should be the primary determinant of surgical intervention rather than absolute numbers of initial or persistent chest tube output. Indications for thoracotomy include evacuated blood volumes exceeding 10-15 mL/kg of blood, blood loss exceeding 2-4 mL/kg/hr, or continued large air leak.5
Massive or a tension pneumothorax may be recognized by decreased breath sounds over the affected lung, jugular venous distension, tracheal deviation opposite the affected lung, and hypotension. Tension pneumothoraces should be suspected clinically and treated emergently with needle decompression prior to imaging.
A massive hemothorax and a tension pneumothorax may be difficult to differentiate clinically, as the signs are similar. Classically, however, a significant hemorrhage causes flat neck veins compared to the distended neck veins associated with a tension pneumothorax. If percussion is performed, hemothorax (dullness) and pneumothorax (hyperresonance) also may be distinguished.
Persistent air leak or pneumothorax despite chest tube drainage and suction or significant hemoptysis should prompt consideration of a tracheobronchial tree injury. CT imaging of the chest is the best, non-invasive study of choice for identifying these injuries. Tracheobronchial tree injuries require operative repair once the patient is stable. (See Table 3.)
Table 3. Blunt Chest Trauma
|
Respiratory distress, inability to oxygenate or ventilate: pulmonary contusion, rib fractures, hemothorax, pneumothorax, tracheobronchial injury, traumatic asphyxia, diaphragmatic injury |
|
Poor perfusion: cardiac injury, great vessel trauma, pericardial tamponade, massive hemorrhage |
|
Muffled heart tones or new murmur: cardiac injury or pericardial tamponade |
|
Facial petechaie: traumatic asphyxiation |
|
Decreased breath sounds: hemothorax, pneumothorax, diaphragmatic rupture |
|
Dullness to percussion: hemothorax |
|
Hyperresonance to percussion: pneumothorax |
|
Decreased breath sounds with mediastinal or tracheal deviation: massive hemothorax or tension pneumothorax |
|
Bubbling at chest wound: sucking chest wound |
Pediatric Cardiac Injury
Pediatric cardiac injury can be significant because of the child’s mobile mediastinum and poor cardiac reserves. Great vessel injury and cardiac rupture, while rare, are often immediately fatal. Those children who do survive initially often are critically unstable and have signs of cardiac contusion (dysrhythmias), pericardial tamponade (hypotension, jugular venous distention, muffled heart sounds), or massive hemothorax. Children with penetrating trauma to the heart or great vessels have a better outcome than those who have blunt rupture. For this reason, a resuscitative thoracotomy in the emergency department is not indicated for victims of blunt chest trauma arriving to the emergency department without a perfusing rhythm. In cases of penetrating trauma, resuscitative thoracotomy has a low but not negligible success rate in patients who arrive with pulseless electrical activity, assuming a surgeon and operating room are immediately available for definitive management.
Abdominal/Genitourinay Trauma
Epidemiology. The most common mechanisms for abdominal injuries in children are motor vehicle collisions, pedestrians struck by motor vehicles, falls, and bicycle accidents. Other less common mechanisms are sports injuries or falls from animals. Although non-accidental injuries, including abuse and assaults, are less common, they are important mechanisms of injury because of the increased risk for severe trauma and high mortality.
Pathophysiology
A child’s lack of subcutaneous fat, anteriorly displaced abdominal organs, and compliant ribs make pediatric abdominal organs more vulnerable to injury. Direct blows to the abdomen, such as from a bicycle handlebar, should raise concern for pancreatic injury or intestinal hematoma/rupture. (See Figure 1.) Abdominal wall trauma from lap belts is associated with a high rate of intra-abdominal injury, including bowel/organ injury, traumatic hernia, or vascular injury. The lap belt syndrome refers to injuries in the area under the lap belt and includes injury to the small and large bowel and their mesentery, trauma to the stomach, liver, spleen, pancreas, kidneys, lumbar vertebrae (Chance fracture), spinal cord injuries, pelvic fractures, and rib fractures.6 Patients with a seat belt contusion commonly have intra-abdominal injuries. Studies have reported that 67-79% of patients had a hollow viscus injury, mostly in the jejunum or ileum.7 The incidence of seat belt injuries has greatly declined with the appropriate use of car seats, booster seats, and shoulder restraints. According to the National Highway Traffic Safety Administration, appropriate use of child restraint devices based on a child’s size reduces the risk of death in children by 71%.8 Recently, Achildi et al reported children involved in motor vehicle collisions who are improperly restrained are at higher risk of sustaining injuries.9 The risk of significant intra-abdominal injuries is increased almost fourfold in these children. Presence of abdominal wall ecchymosis (AWE) was associated with intra-abdominal injuries in up to 84% of children, with hollow viscus injury being the most common. Likewise, presence of AWE is associated with vertebral fractures, including Chance fractures, in up to 50% of patients. Vertebral fractures were associated with spinal cord injury in up to 11%. The presence of AWE in an improperly restrained child should warrant a thorough search for intra-abdominal injuries, vertebral fractures, and spinal cord injury.10
Figure 1. Handlebar Sign

Clinical Presentation
Children with abdominal injuries typically have abdominal pain, bruising, and/or tenderness. Taylor et al found that mechanism of injury, revised trauma score ≤ 12, abdominal tenderness, abdominal distention, absent bowel sounds, fractured pelvis, gross hematuria, chest trauma, and hematocrit < 30% were all associated with abnormal CT scans.11 In a prospective study of 1,095 children, Holmes et al12 found that low blood pressure, abdominal tenderness, femur fracture, hematocrit < 30%, alanine aminotransferase (ALT) > 125 U/L and/or aspartate aminotransferase (AST) > 200 U/L, and urinalysis with > 5 RBC/hpf (red blood cells per high power field) were significantly associated with abdominal injuries on CT scan.
Diagnostic Evaluation
A retrospective series of the use of a trauma panel in children showed that no single laboratory screen was clinically significant for abdominal pathology.13 Increased AST and ALT levels, in addition to microscopic hematuria and an abnormal physical examination, may be associated with an intra-abdominal injury. Elevation of glucose and white blood cell count may occur as a stress response to the trauma and does not correlate with injury severity.
Hematuria is helpful for the identification of serious renal and non-renal trauma in children. Hynick et al found that hematuria (gross or microscopic), elevated serum ALT, and documentation of clinically concerning abdominal findings upon examination remained significant predictors (odds ratio [OR], 3.5; 95% confidence interval [CI], 1.8-6.8; OR, 10.9; 95% CI, 2.5-47, respectively) of a clinically important injury.14
Streck et al found four variables were identified as significant individual predictors of intra-abdominal injury: elevated AST, decreased hematocrit, abnormal abdominal exam, and abnormal chest X-ray.15 An elevated AST
(> 200) was seen in 68.8% of patients with intra-abdominal injury and potentially represents a liver injury or ischemia and should increase suspicion for serious intra-abdominal injury. A low HCT (< 30) was seen in 29.4% of patients with identified intra-abdominal injury. Abnormal abdominal exam was seen in 76.5% of patients with intra-abdominal injury and should prompt further evaluation. The sensitivity of abdominal examination may be limited in patients with young age, distracting injuries, or decreased levels of consciousness. A fourth variable that seemed useful in this study population was abnormal chest X-ray, which was seen in 58.8% of patients with intra-abdominal injury. (See Table 4.)
Table 4. Diagnostic Evaluation
Laboratory Test |
Indications |
|
CBC and Blood Type and Screen |
Suspected spleen or liver laceration, hollow viscus injury, or vascular injury |
|
Blood Type and Cross Match |
Obvious or suspected external or internal bleeding, positive FAST, or hypotension |
|
Serum Electrolytes, Lipase, Transaminases |
Suspected liver or pancreatic injury (AST levels > 450 IU/L and/or ALT levels > 250 IU/L; lipase > 200 IU/L) |
|
Urinalysis |
Gross hematuria, significant trauma to the abdomen or flank concerning for renal injury |
Plain Radiographs. Plain radiographs typically are not useful for the evaluation of a child who has sustained blunt abdominal trauma. In children with peritoneal signs or penetrating trauma, however, plain radiographs may be useful for the detection of free intraperitoneal air (i.e., bowel perforation) and the need for emergent surgical intervention. Streck et al found an abnormality on chest X-ray, particularly a rib, clavicle, or scapular fracture, likely represents a high severity of blunt force to the torso, as the bony skeleton in children is more compliant.15 This degree of force, coupled with the relative lack of coverage of internal organs by the skeleton (relatively larger liver, more intra-abdominal than pelvic bladder), significantly increases the likelihood of underlying intra-abdominal injury.
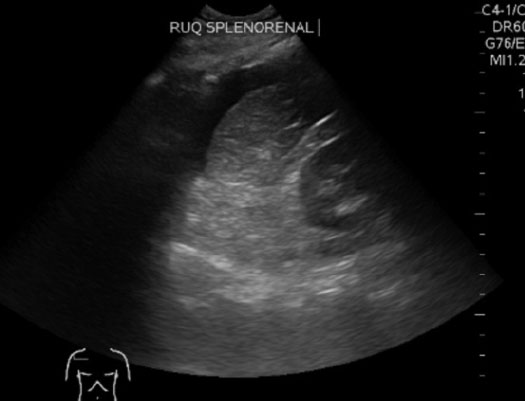
Ultrasound. The Focused Assessment with Sonography for Trauma (FAST) exam has become a useful part of the initial trauma evaluation. FAST evaluates for free intraperitoneal and pericardial fluid, which usually represents hemorrhage in the setting of trauma. A bedside FAST exam is indicated in all blunt and penetrating abdominal trauma. Views include pericardiac, perihepatic, perisplenic, and pelvic windows (known as the 4 Ps). It can be performed quickly during an ongoing resuscitation, is noninvasive and portable, may be repeated multiple times if indicated, and does not offer a radiation dose. In the hands of a skilled and experienced operator, the FAST exam can reliably detect as little as approximately 200 mL of intraperitoneal fluid.
A recently published meta-analysis included 25 studies using the FAST exam in pediatric blunt trauma. Ultrasound had a sensitivity of 80% (76-84%) and a specificity of 96% (95-97%) for the identification of hemoperitoneum.12 Hemodynamically stable patients with positive FAST findings may require a CT scan to better define the nature and extent of injuries. Unfortunately, ultrasound does not identify all intra-abdominal injuries, making abdominal CT necessary for patients with clinical suspicion for injury and a negative FAST exam. In hemodynamically unstable patients, a positive FAST examination suggests the need for a laparotomy, while a negative FAST examination should suggest there may be an extra-abdominal source of blood loss. In hemodynamically stable patients, an abdominal CT should be done on patients with a positive FAST examination to better define the injury. If the FAST is negative, the patient can be followed with serial examinations for six hours and a follow-up ultrasound or abdominal CT scan. (See Figure 2.)
Figure 2. Positive FAST Exam in Splenorenal Recess
Abdominal/Pelvic CT Scan. CT remains the gold standard for diagnosing abdominal injuries. Radiation should be kept “As Low As Reasonably Achievable (ALARA).” CT scans should be performed only when medically necessary and when the results will likely influence the management of the patient. (See Table 5.) Identifying children at very low risk of serious intra-abdominal injuries in whom imaging is not indicated remains difficult.14 One study indicated that abdominal tenderness, femur fracture, elevated serum AST (> 200 units/L) or serum ALT (> 125 units/L), or a urinalysis with at least 5 RBC/hpf was associated with an increased incidence of intra-abdominal injuries.15 Taylor et al also attempted to identify indications for abdominal and pelvic CT scanning for traumatized children.11 Findings associated with intra-abdominal injuries in this study included abdominal tenderness, lap belt injury, gross hematuria, and assault or abuse as the mechanism of injury. Children with gross hematuria should have an abdominal/pelvic CT performed to assess for renal trauma. Cystourethrography is indicated in stable patients with suspected lower genitourinary tract injury. In addition to solid organ injuries, children are more prone to intestinal, pancreatic, and mesenteric injuries, which are not always readily apparent on laboratory or imaging evaluation. In addition, the FAST exam and even CT imaging will frequently miss these injuries. Therefore, serial abdominal examinations are a mainstay of evaluation and management of pediatric blunt abdominal trauma. For a summary of markers of abdominal injury and indications/contraindications for pediatric abdominal and pelvic CT scan, see Tables 5 and 6.
Table 5. Indications for Pediatric Abdominal and Pelvic CT Scan
Reasonably Well-supported Indications
- Intubated children undergoing mechanical ventilation
- Altered mental status
- Children with spinal cord injuries resulting in loss of abdominal sensation
- Gross hematuria
- Abdominal tenderness
- Persistent complaints of abdominal pain
- Free fluid on bedside ultrasound FAST examination
- Abdominal or flank bruising
- Suspected non-accidental trauma to the abdomen
- Seat belt mark above the iliac crests
- Direct blow to the abdomen from bicycle handlebars or kicking
Controversial Indications
- Microscopic hematuria
- Elevated liver transaminases
- Isolated femur fracture
- Preverbal children with mild-to-moderate injuries
Resasonably Well-supported Contraindications
- Persistent hemodynamic instability despite adequate fluid resuscitation* (especially in the setting of a positive FAST scan) — in this case, bypass CT and go to the operating room
* What constitutes “adequate” fluid resuscitation has not been satisfactorily defined.
Table 6. Markers of Abdominal Injury
Abdomen
- Bicycle handlebar injury or elevated lipase: pancreatic injury (can be isolated)
- Seat belt sign or lumbar fracture: intra-abdominal injury common
- Kehr’s sign (left shoulder pain with left upper quadrant palpation): referred pain indicative of splenic injury
- Elevated liver enzymes: possible hepatic injury
- Persistent bilious emesis: duodenal hematoma or pancreatic injury
- Peritonitis: hollow viscus injury
- Free air on upright radiograph: hollow viscus injury or penetrating abdominal wall trauma
- Positive Focused Assessment Sonography in Trauma (FAST): hemoperitoneum; possible splenic or hepatic injury; indication for CT abdomen/pelvis if hemodynamically stable or emergent exploratory laparotomy if hemodynamically unstable
- Back pain: possible retroperitoneal injury
Pelvis/Genitourinary
- Hematuria: urethral, bladder, or renal injury; possible pelvic fracture
- Blood at the urethral meatus: ureteral injury
Diagnostic Peritoneal Lavage. Diagnostic peritoneal lavage is rarely performed, but may be considered for patients who cannot be transported to the radiology suite because of hemodynamic instability or if CT and FAST are not readily available.
Management
As with any traumatic patient, ED providers should perform rapid and early assessment and management of the primary survey principles. If there are signs or symptoms of pneumothorax or hemothorax, consider chest tube placement early. Peripheral venous access should be obtained, and, if unsuccessful, an intraossesous line should be considered. Appropriate dosing of medications and fluids and proper equipment size should be estimated with a length-based tape, such as the Broselow® pediatric emergency tape. The patient should be completely undressed, and the secondary survey should be performed. Bedside ultrasonography should be performed early to identify free fluid in the abdomen, pericardial effusions, pneumothorax, and pleural effusion.
Initial management should be based on the patient’s hemodynamic status. Patients with tachycardia and poor perfusion should be treated immediately with a 20 mL/kg IV bolus of crystalloid solution followed by reassessment and repeat fluid boluses if signs of shock persist. Patients who fail to respond to 40 mL/kg of crystalloid should receive a transfusion of 10 mL/kg of packed red blood cells and receive an emergent surgical consultation for possible operative management.
If the pediatric patient is hemodynamically unstable and has evidence of hemoperitoneum on bedside FAST exam, emergent laparotomy is indicated. If stable, screening laboratory studies may suggest liver injury (increased transaminase levels), genitourinary injury (gross hematuria), pancreatic injury (increased lipase levels), or bowel ischemia/poor perfusion/shock (elevated lactate levels). CT imaging should be performed to identify specific injuries. (See Figure 3.)
Figure 3. CT Scan Showing Liver Laceration and Right Perinephric Hematoma

Nonoperative management of many blunt intra-abdominal solid organ injuries is appropriate in hemodynamically stable children. The grade of splenic or hepatic injury does not mandate immediate surgical intervention, as hemorrhage associated with these injuries is usually self-limited. Close observation and monitoring by a qualified surgeon in a pediatric intensive care unit with serial hemoglobin/hematocrit monitoring may obviate the need for invasive surgical intervention. This may be best performed in a pediatric trauma center.
National Guideline/Academic Resource
REFERENCES
- Ten leading causes of death and injury. Available at www.cdc.gov. Accessed July 20, 2016.
- Cooper A, Barlow B, DiScala C, et al. Mortality and truncal injury: The pediatric perspective. J Pediatr Surg 1994;29:33-38.
- Nakayama DK, Ramenofsky ML, Rowe MI. Chest injuries in childhood. Ann Surg 1989;210:770-775.
- Notrica DM, Garcia-Filon P, Moore FO, et al. Management of pediatric occult pneumothorax in blunt truama: A subgroup analysis of the American Association for the Surgery of Trauma multicenter prospective observational study. J Pediatr Surg 2012;47:467-472.
- Avarello JT, Cantor RM. Pediatric major trauma: An approach to evaluation and management. Emerg Med Clin North Am 2007;25:803-836.
- Santschi M, Lemoine CL, Cyr D. The spectrum of seat belt syndrome among Canadian children: Results of a two-year population surveillance study. Paediatr Child Health 2008;13:279-283.
- Santschi M, Echave V, Cyr C. Seat-belt injuries in children involved in motor vehicle crashes. Can J Surg 2005;48:373-376.
- Kahan CJ. An evaluation of child passenger safety: The effectiveness and benefit of safety seats. NHTSA Report Number DOT HS 806 890. Available at: NHTSA.gov. Accessed July 20, 2016.
- Achilda O, Betz RR, Grewal H. Lapbelt injuries and the seatbelt syndrome in pediatric spinal cord injury. J Spinal Cord Med 2007;30 (supp 1):S21-S24.
- Eberhardt CS, Zand T, Ceroni D, et al. The seatbelt syndrome — Do we have a chance? A report of 3 cases with review of literature. Pediatr Emerg Care 2015 Jun 17. [Epub ahead of print].
- Taylor GA, Eichelberger MR, O’Donnel R, et al. Indications for computed tomogrphy in children with blunt abdominal trauma. Ann Surg 1991;213:212-218.
- Holmes JF, Mao A, Awasthi S, et al. Validation of a prediction rule for the identification of children with intra-abdominal injuries after blunt torso trauma. Ann Emerg Med 2009;54:528-533.
- Keller MS, Coln CE, Trimbloe JA, et al. the utility of routine trauma laboratories in pediatric trauma resuscitations. Am J Surg 2004;188:61-68.
- Hynick NH, Brennan M, Schmidt P, et al. Identification of blunt abdominal injuries in children. J Trauma Acute Care Surg 2014;76:95-100.
- Streck CJ, Jewett BM, Wahlquist AH, et al. Evaluation for intra-abdominal injury in children following blunt torso trauma. Can we reduce unnecessary abdominal computed tomography by utilizing a clinical prediction model? J Trauma Acute Care Surg 2012;73:371-376.
Trauma patients are often very difficult to assess, particularly young children.This article reviews trauma in children. It reminds us that children are not little adults. Their injury pattern and their response to injury are unique.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
