The pediatric abdominal trauma patient presents a unique challenge to the acute care provider. The history may be difficult to obtain, not only because the child may not be able to provide any information, but because parental anxiety and concern may cloud the details. A recent surge of literature regarding pediatric abdominal trauma, with particular interest in the diagnostic evaluation needed to fully evaluate the child, has emerged. Key laboratory studies and reducing radiation exposure have become a focus. The safety of close observation vs. exploratory surgery in solid organ injuries is being explored, showing that the operating room may not always be the right choice. This article will cover major points the provider needs to know to appropriately manage a child with potential abdominal trauma, including the acute resuscitation and specific organ injury management.
— The Editor
Introduction
Trauma is the leading cause of death and disability in children.1 In 2011, more than 8 million children younger than 15 years of age were seen in U.S. EDs for the assessment and treatment of injuries.2 Those visits accounted for almost 35% of that year’s ED volume.3 More than 40% of the incidents that led to these ED visits occurred around the home.4 Unintentional falls are the most common mechanism of nonfatal injury among children, and motor vehicle collisions (MVCs) are the most common cause of death.3
Abdominal trauma constitutes 10-15% of the injuries seen in pediatric trauma patients.5 This type of trauma is the most common unrecognized cause of trauma-related deaths. Approximately 90% of abdominal trauma is blunt and 10% is penetrating.3 Blunt abdominal trauma is the third most common cause of pediatric trauma-related deaths.3,6 The spleen and liver are the most frequently injured organs, followed by the kidney, small bowel, and pancreas. The most common mechanisms of injury are MVCs, pedestrians struck by vehicles, car vs. bike, and falls, followed by contact with bike handlebars, sports, incidents involving all-terrain vehicles or furniture, and nonaccidental trauma (NAT).3
Evaluating children with trauma might not be as simple or occur as frequently as assessments of adult trauma patients. A child’s body structure is different from that of an adult, responds differently to stress, and undergoes various developmental stages that can present a challenge.3 When faced with an injured child, the physician needs to know not only the cause of the trauma to evaluate the injury, but also, at the same time, must recognize that traumatic injury to a child might not have the same presentation or treatment as the same injury in an adult.
Elucidating the mechanism of injury is just the first step in the evaluation to determine if the risk of abdominal trauma is present. Pediatric patients require weight-based resuscitation. Care must be taken to decide which laboratory tests are necessary and if radiation exposure is needed to determine the extent of injury. Once the patient has been resuscitated and injuries have been identified, the pediatric abdominal trauma patient needs to be at a center with the appropriate resources.
Physiology
Children are anatomically different from adults. Children have relatively larger abdominal organs that are surrounded by less fat and less developed abdominal musculature.6,7 The liver and spleen are more anterior, making them more prone to injury than those organs in adults.8 The rib cage is more compliant, allowing greater transmission of force to underlying organs such as the kidneys, liver, and spleen.7,9 Body mass is smaller in a child, yielding a greater force per unit of body surface area.9 This force is then easily transmitted throughout the entire body, leading to more significant injuries, possibly without external signs.9 Children also have a larger body surface area than adults, putting them at increased risk of hypothermia.6,9 Energy requirements and glucose consumption per kilogram are higher as well.6
Aside from body structure, children also differ from adults physiologically. Most importantly, pediatric patients compensate for blood loss differently than adults do. A normal blood pressure on presentation should not be a reassuring sign that the child has no injuries. Children initially compensate for hypovolemia by increasing their heart rate. Later findings of significant hemorrhage are weakening peripheral pulses, a decrease in pulse pressure to less than 20 mmHg, mottling, cool and clammy skin, and a decreased level of consciousness.9 The blood pressure will not change until approximately 30% of the blood volume has been lost.6,9 Reliance on capillary refill alone as a proxy for intravascular volume could give false reassurance.
Penetrating Trauma
Penetrating trauma in children is much less common than in adults.3,10 It accounts for less than 3.6% of hospital admissions.4 Most penetrating injuries are caused by shootings and stabbings, generally in older children. However, common household objects also may serve as penetrating objects. There have been case reports of significant abdominal trauma inflicted by a frying pan, a storm door, an umbrella, and broken glass.4
Gunshot wounds present a unique challenge in that they are not a single linear injury. The high kinetic energy of bullets, along with explosive gun particles and blast effect, can change the route of the bullet after it enters the body, increasing damage along its path. Secondary fragmentation causes additional injuries as well.11
With regard to penetrating abdominal trauma, the small bowel is injured more often than the large bowel, which is injured more often than the liver. The risk of complications can be predicted by clinical shock, the number of organs injured, the amount of blood transfusions needed, and concomitant thoracic trauma.11
While exploratory laparotomy is currently considered the gold standard for management of pediatric patients with penetrating abdominal trauma, recent studies are showing that minimally invasive laparoscopic surgery can be used in the hemodynamically stable patient. This approach may decrease morbidity and mortality associated with exploratory laparotomy. However, some authors believe that laparoscopic surgery in the setting of penetrating trauma could miss damage to the solid organs, small bowel, mesentery, ureters, and bladder.12 Ongoing research also is looking at possible nonoperative management of specific penetrating injuries in patients who are hemodynamically stable without signs of peritonitis.11 In one study involving patients with penetrating abdominal and thoracic trauma (from shootings or stabbings), 36% of children went to the operating room while 64% were managed conservatively, with no poor outcomes noted.10 Conservative management of penetrating abdominal trauma in the pediatric population is a newer area of research; this type of management has been more established in blunt abdominal trauma.
Blunt Trauma
Motor Vehicle Collisions. In 2010/2011 in the United States, there were 537.4 MVC-related ED visits per 10,000 patients.13 Optimally restrained children younger than 16 years of age were three times less likely to have an abdominal injury than unrestrained passengers.14 The use of a lap/shoulder belt by children older than 5 years of age reduced mortality by 45% and morbidity by 50%.13 In 2011, the American Academy of Pediatrics revised its seatbelt recommendations to include rear-facing car safety seats for most infants up to 2 years of age, forward-facing car safety seats through 4 years of age, belt-positioning booster seats for most children through 8 years of age, and lap/shoulder seat belts for all who have outgrown booster seats. It is recommended that all children younger than 13 years ride in the rear seat of a vehicle.16 The improper use of a two-point seatbelt or the improper use of a three-point restraint causes increased flexion/distraction injuries from a baseline 5.1% to 66.7%, leading to more compression-based injuries.17 Children aged 5 to 9 years are most susceptible to abdominal injuries due to the higher rate of noncompliance with the booster seat.17 No reduction in the prevalence of abdominal injury was found when rear- vs. front-facing car seats were tested in this age group.18 It is important to note that side impact is associated with a higher rate of abdominal injuries than frontal impact.19 When evaluating a child after a car crash, it is imperative to ask how the incident occurred, where the car is damaged, and what type of restraint was used.
After a significant collision, the car seat needs to be replaced, even if there is no evidence of any damage to the seat. The National Highway Traffic Safety Administration recommends mandatory replacement of a car seat after a moderate or severe collision. After a minor collision, the seat does not automatically require replacement. A minor crash meets all of the following criteria: the vehicle was able to be driven from the crash site, the door nearest the safety seat was not damaged, there were no injuries to anyone in the vehicle, no airbags were deployed, and there was no visible damage to the car seat.20 Although this information may not be needed while resuscitating the patient, it is an important piece of information to relay to a caregiver in preparation for discharge of the patient.
Although seatbelts were designed to protect passengers from devastating injuries, the restraint itself might cause injury while preventing more significant injury that could occur if the passenger was unrestrained. Seatbelt syndrome (erythema, ecchymosis, or abrasions across the abdominal wall) was first reported in children in the 1980s.15 The seatbelt lies over the abdomen, and a sudden deceleration bends the child around the lap belt.17 This sign is seen in 1-10% of MVCs.6,17 Intra-abdominal injuries are more common in patients with the seatbelt sign than in those without, and its presence is an independent predictor of an intra-abdominal injury that needs acute intervention.15 The mesentery, bowel, and pancreas are most commonly injured. If a seatbelt sign is present, the rate ratio is 2.9 for any intra-abdominal injury, 12.8 for gastrointestinal injury, and 22 for pancreatic injury.21 However, no increased risk of solid organ injury has been identified.15 Spinal injury is present in half of the patients with this sign.17 A seatbelt sign signifies a significant force was transmitted to the abdomen and requires further investigation.
Pedestrian Struck by a Vehicle. Children are more vulnerable than adults to being struck by a vehicle. Those at higher risk include younger children, males, children with lack of parental supervision, and those with impulsivity. While there is a higher incidence of pedestrians being struck by a vehicle in urban settings, more fatalities occur in rural areas. The classic Waddell Triad (damage to the head, legs, and abdomen) occurs in approximately 2.4% of children struck. Injury patterns depend on vehicle speed, angle of impact, the victim’s center of gravity, vehicle contact point, the body part that contacts the vehicle, and the vehicle’s design.3 The receiving physician should ask prehospital care providers for information about the car, if known, and the point of contact between the car and the child.
Falls. In 2010/2011 in the United States, falls accounted for 661.9 of 10,000 ED visits by children younger than the age of 18 years.13 Falls are an exceedingly common nonfatal injury in children younger than 15 years. The majority occur in private homes. One study showed that 4% of children who fell had an intra-abdominal injury. Abdominal injuries were equally likely to occur in falls less than 15 feet as in those greater than 15 feet, but the injuries from the greater height were more severe.22 It is important to note that intra-abdominal injuries were not found to be associated with falls down stairways.23
Bicycle Incidents. Bicycle crashes are the leading cause of sports-related ED visits for children in the United States, many of them for boys between 10 and 14 years of age. The mortality rate from bike incidents is comparable to the overall mortality from pediatric trauma.7 One study of 219 children showed that liver laceration was the most common intra-abdominal injury, followed by damage to the pancreas and the hollow viscus.24,25 Kidney injury and abdominal wall hernias also can occur.25 A study by Teish et al, conducted over 12 years at a Level I trauma center, showed that 80 patients were admitted after being injured in bicycle crashes, accounting for 4% of all trauma admissions during the study period. Seventeen of the 80 patients (21%) had intra-abdominal injuries. Twenty percent of the children younger than 6 years of age required operative intervention. The younger the child, the more likely that operative intervention was required.7
Ten percent of bicycle injuries are related to contact with handlebars.24 Handlebars are 10 times more likely to be the cause of severe injury than other causes of bicycle-related trauma. (See Figure 1.) Half of handlebar injuries are misdiagnosed initially.3 Handlebar injuries are complicated by the fact that the patient might not have any skin marking,25 and clinical presentation often is delayed.3 In 2001, a bike with retractable handlebars with a spring mass damper system was designed. It was postulated that this could decrease the force of abdominal impact by 50% and would thereby decrease the number of abdominal injuries.7 This design never gained popularity. In a Canadian study, more than 50% of patients who sustained blunt impact to the abdomen from handlebars or a direct blow had at least one notable injury.26 Patients with isolated bicycle handlebar injuries, a negative Focused Abdominal Sonography in Trauma (FAST) exam, normal laboratory results, and clinical improvement over 24 hours are safe for discharge.25
Figure 1. Handlebar Sign

Image courtesy of Aaron Leetch, MD.
Contact Sports. According to the National Pediatric Trauma Registry, 0.56% of abdominal injuries are sustained during participation in contact sports. In Australia, rugby leads to the most abdominal injuries, followed by soccer, cricket, and baseball. In the United States, the sports most responsible for these injuries are football, hockey, baseball, soccer, and basketball.3 The spleen is the organ most often injured, followed by the kidney and liver. Infectious mononucleosis can cause an enlarged spleen, which can predispose a person to splenic rupture. Infectious mononucleosis can present nonspecifically with symptoms including malaise, fatigue, and pharyngitis. In athletes, it is important to maintain a high level of suspicion for infectious mononucleosis when a patient presents with these vague symptoms since the risk of splenic rupture is the highest within the first 21 days after illness. The risk of splenic rupture is < 0.5%, but the sequelae are severe. Most guidelines for return to play are tailored to individual players. Ultrasound may be used to assess splenomegaly, but the utility is limited by a baseline variability in spleen size. Most players will be able to return to play in 28 days.27
Nonaccidental Trauma. According to the Centers for Disease Control and Prevention (CDC), NAT is the fifth leading cause of death among children younger than 1 year of age in the United States.1 The annual prevalence of NAT is 2.33 cases per million children younger than 5 years of age and 0.9 cases per million children of all ages. Abdominal trauma contributes to up to half of the deaths of abused children.8 It is the second most common cause of death (superceded by head injuries) from child abuse. The morbidity and mortality associated with abdominal injuries resulting from NAT are higher than those associated with accidental abdominal trauma.3 The mortality rate from NAT is 53% compared to 21% for accidental trauma.8
Abused children are typically younger than their unintentionally injured counterparts.8 They are more likely to have a delayed presentation and require surgical intervention.3,8 As few as 12% of children with inflicted abdominal injuries have bruising.8
The organs most commonly affected by NAT are the liver and small bowel.8 Hollow viscus injury is more likely to occur in NAT patients compared to accidentally injured children. Intentional injury is the leading cause of intestinal perforation in children who have sustained blunt abdominal trauma.3 The most common sites of perforation are the third and fourth portions of the duodenum. Liver injuries occur in equal measure among children involved in abusive and nonintentional incidents.8 During the ED assessment, if the concentration of either transaminase (aspartate or alanine) is found to be higher than 80 IU/L, CT with intravenous contrast is recommended.28 This value is specific to NAT.
Duodenal hematomas typically do not occur accidentally in children younger than 4 years of age; suspect NAT. Small bowel injuries are not seen as a result of accidental falls in children younger than 5 years of age. These injuries should raise suspicion for NAT.8 The mechanism of injury needs to match the pattern of injury on the patient; if it does not, then NAT should be considered. The prehospital team should be aware of circumstances that might be suspicious for NAT, but they should never make an accusation on the scene.
Prehospital Care
When an injured child is encountered in the prehospital setting, considerations first need to go to assessment of the child as a whole: the primary and secondary survey, identification of immediate threats to life, assessment of vital signs, and pain control. While local emergency medical services (EMS) off-line protocols can provide basic guidance, on-line medical control may provide an additional resource. EMS field guidelines published by the CDC outline scenarios that warrant transfer to a trauma center. These include physiologic signs (Glasgow Coma Scale [GCS], systolic blood pressure, respiratory rate), anatomic criteria (including central penetrating trauma or multiple long bone fractures), and criteria based on mechanism of injury (compartmental intrusion or significant falls) or age. There is also a section that allows for provider discretion.29
One important consideration is to ensure that the child is taken to an appropriate facility. Field decision trees allow up to 70% over triage. Nabaweesi and colleagues found that a GCS less than 9, an abnormal heart rate, and associated chest trauma correlated with full trauma team activation and disposition to the intensive care unit, operating room, or morgue.30 While a child’s elevated heart rate may be due to anxiety and fear rather than the injury, the prehospital team should err on the side of caution. Hospitals that see pediatric trauma patients more frequently are better equipped to handle severely injured children.
Emergency Department Management
When facing the resuscitation of a pediatric patient, the healthcare provider often has to interact with and try to assure a distraught parent or caregiver. In certain circumstances, a parent or other family member can be helpful in calming the child and providing information about the child’s history, but if they are distressed, they can increase the child’s anxiety. It may be helpful to have a second person dedicated to the parent. The child’s history is fundamental to the ED evaluation, but it can be difficult to obtain for a variety of reasons. A knowledgeable adult might not be present, the patient might be too young to describe what has happened, or the patient may be trying not to get in trouble.3 If the patient presents via ambulance, emergency service personal often are able to provide additional history, important information about how the incident scene looked on arrival, abnormal vital signs, and any interventions that they provided, such as fluid administration or pain control.
For the patient with suspected abdominal trauma, the assessment should begin as with any pediatric trauma. Primary assessment starts with the ABCDEs (airway, breathing, circulation, deficit or deformity, exposure). The child should be fully exposed while being careful to avoid hypothermia. Remember to use age-adjusted vital signs and an appropriate weight. A length-weight based tape is useful for determining the weight and appropriate medication dosing. Start with administration of a 20 mL/kg bolus of an isotonic solution in any patient with tachycardia or poor perfusion with a concern for intra-abdominal injury. If the patient remains unstable after the first fluid bolus, surgical consultation should be obtained. Continue fluid resuscitation with two additional 20 mL/kg boluses of an isotonic solution as needed.9 As a caveat, increased administration of prehospital crystalloid was associated with an increased blood transfusion requirement, prolonged prothrombin time, and a tendency toward increased organ failure and mortality.31 If the patient is still unstable or is deteriorating, administer 10 mL/kg of packed red blood cells.6 In the unstable trauma patient, make sure to consider early administration of blood products, especially if there is continued bleeding or the patient remains unstable after crystalloids.
Early administration of a balanced ratio of red blood cells, fresh frozen plasma, and platelets shows improved outcomes in adults with massive hemorrhage.31 Massive bleeding in pediatrics is defined as a loss of more than 70 mL/kg in patients older than 3 months.31 Massive transfusion protocols have not yet proven to be beneficial in pediatrics.32,33 A higher plasma or platelet to red blood cell ratio has not been associated with increased survival in pediatric patients receiving a packed red blood cell transfusion of more than 50% total blood volume.34 In one study only involving children, having a massive transfusion protocol compared to physician discretion showed no difference in mortality.31,35
Key resuscitation points specific to the abdomen include decompression with a nasogastric or orogastric tube for abdominal distension if this procedure is not contraindicated. A Foley catheter also should be placed if the patient is hemodynamically unstable or if input and output need to be monitored closely.5,6 Contraindications for Foley catheter placement include high suspicion of a urethral injury. This could be indicated by blood at the urethral meatus. If a urethral injury is suspected, urology should be consulted for a retrograde urethrogram prior to catheter insertion.
The abdominal examination provides essential information for determining whether further evaluation is needed. First, observe the abdomen, looking for any bruising, abrasions, or distension. A seatbelt sign should raise concern for intra-abdominal injury. Kehr’s sign suggests splenic injury, and flank bruising could indicate retroperitoneal bleeding.6 Next, listen for bowel sounds. The absence of bowel sounds in the presence of peritonitis and abdominal distension is associated with intra-abdominal injury.36 While the stethoscope is still on the patient’s abdomen, it can be used to gently palpate for tenderness, rebound, or guarding while the child does not realize that light pressure is being applied.
Intra-abdominal injury is likely present in patients with generalized abdominal pain and tenderness. In the group studied by Adelgais et al, the sensitivity for abdominal pain in detecting acute pathology was 79% in patients with a GCS score of 15 and dropped to 32% in patients with a score of 13.36 The lower the GCS score, the more likely that an intra-abdominal injury is present. With a score of 15, the rate of intra-abdominal injury without abdominal pain or tenderness was only 2%. If patients have isolated abdominal pain or tenderness on examination, the rate of intra-abdominal injury is 8%, with 1% needing an acute intervention such as blood transfusion or surgery. A rectal exam is not routinely indicated for patients with abdominal trauma. Adelgais and colleagues found no association between the detection of blood on the rectal examination and intra-abdominal injury.36
During the assessment of an injured child, the abdomen will probably be examined by several practitioners. Yen et al showed that they can achieve an acceptable level of agreement based on the history and physical exam. Physicians tend to agree on the presence of abdominal tenderness, abdominal wall trauma, and abdominal distension, but not peritonitis.37
Every patient needs to have his or her pain assessed, treated, and re-evaluated. Throughout the past decade, research has shown that pain management in children, in both the prehospital and the hospital setting, is in need of improvement. Studies looking at pain management have shown no difference in mortality or disposition on discharge with regard to analgesia timing.38 Barriers to administration of analgesia include the myth that neonates do not experience pain, the assumption that children experience less pain than adults, a lack of knowledge, an inability to assess pain, and the fear of side effects of analgesic medication.39,40 There is a large amount of literature in pediatrics examining the safety and effectiveness of several pain medications such as morphine and fentanyl. Various delivery systems, including intravenous, intramuscular, and intranasal administration, also have been shown to be efficacious.41 During a trauma resuscitation, the patient’s hemodynamic stability and the typical side effects of a pain medication should be given due consideration.
Children are given pain medications less commonly than adults for the same type of trauma. Presentation to a Level I trauma center, trauma team activation, and parental preference lead to more common use of analgesia. In a retrospective study examining pain medication use in pediatric trauma, Anantha et al found that only 32% of pediatric trauma patients received analgesia. Patients who were injured in MVCs or placed in a resuscitation room were more likely to receive pain medication.38 While actively resuscitating patients, care should be taken to assess and treat pain.
Laboratory Evaluation
Once venous access is established, blood samples can be obtained. In the critically ill or penetrating trauma patient, blood work should include a complete blood count (CBC), complete metabolic profile (CMP), and type and screen. Urinalysis (UA) should be requested as well. If alcohol or other toxidromes are suspected, then toxicology screens also should be performed. Obtain a pregnancy test in patients of childbearing age.6
Only those labs that are needed should be drawn. If the patient is not critical and has isolated abdominal trauma, then the labs ordered should be specific for indicating intra-abdominal injury. For the hemodynamically stable patient for whom suspicion is still high for abdominal trauma, several screening blood tests have been shown to be beneficial in diagnosis. Elevated transaminases (aspartate aminotransferase [AST] > 200 IU/L or alanine aminotransferase [ALT] > 125 IU/L) and UA indicating microscopic hematuria are the best predictors of intra-abdominal injury.42-46 The absolute number of red blood cells per high power field (RBC/hpf) remains controversial and some early studies have suggested using cutoffs of 5, 10, 20, or 50 RBC/hpf.43-46 A study by Stakler et al showed that in normotensive patients, no significant renal injuries were detected when patients had less than 50 RBC/hpf. When significant renal injury was present, the patient was hemodynamically unstable or with a larger amount of hematuria.46
Obtaining a hematocrit on admission can be helpful in predicting the need for transfusion. In a study by Golden et al, a hematocrit of 35% or less identified children with blunt trauma who would need transfusion, with a sensitivity of 94% and negative predictive value of 99.9%.30 A hematocrit less than 30% is considered a high-risk indicator for injury.47,48 Measuring the hematocrit at this time also serves as a baseline value if the patient requires hospitalization.
The white blood cells (WBCs) may be elevated in patients with intra-abdominal injury, but the term “elevated” has not been defined.48 Hershkovitz et al found that a WBC > 14,000/μL correlated with a positive abdominal CT scan when seen in conjunction with anemia and hematuria.48 Amylase and lipase are not useful predictors of pancreatic injury at initial presentation.6,28 In patients who are hemodynamically stable, with low or moderate concern about intra-abdominal injury, the minimum set of laboratory tests should be measurement of hematocrit, AST, ALT, and UA.
Radiography
Adult trauma resuscitation algorithms have emphasized routine use of screening chest and pelvic radiographs.49 Selective pediatric radiography may be warranted, leading to less radiation exposure and less cost.50 For the blunt abdominal trauma patient, a chest radiograph should be ordered only if there is suspicion of significant associated thoracic trauma, rib fractures, diaphragmatic injury, or pneumothorax.5
Pelvic fractures occur in less than 4% of blunt pediatric trauma patients. A pelvic radiograph is not routinely warranted in the pediatric abdominal trauma patient. The clinical exam has been shown to be reliable in children. Lagisetty et al developed a screening tool for pelvic fracture with a negative predictive value (NPV) of 99% and a sensitivity of 96%.49 Radiograph is not incidated if the answer is “no” to all of the following: pelvic tenderness, laceration, ecchymosis or abrasion over the pelvis; GCS < 14; hematuria, abdominal pain or tenderness, femur fracture; or if the patient was involved in an MVC rollover, MVC with ejection, or was an unrestrained passenger in an MVC, or car vs. pedestrian or bike.49 Haasz et al also developed a set of criteria that, when negative, have a risk rate of less than 0.05% for pelvic fracture. These criteria include: no pelvic pain, normal exam of the hip and pelvis, no femur deformity, no hematuria, no abdominal pain or tenderness, GCS > 14, and stable hemodynamics.51 Pelvic fractures are a high-energy mechanism and are commonly associated with intra-abdominal injuries.50 If the suspicion for pelvic fracture is high, then a radiograph should be obtained, but there is no evidence to support its use as a screening exam.
Focused Assessment with Sonography for Trauma Examination
FAST has become widely integrated into the adult trauma algorithm, but there has been hesitance about its widespread use in pediatric trauma. The Advanced Trauma Life Support guidelines state that the FAST exam is comparable to diagnostic peritoneal lavage in adults but are vague about its use in children.9,52 A 2009 survey revealed that only 15% of pediatric trauma centers used the FAST exam compared with 96% of adult centers.53,54 Advantages to FAST include that it can be done at bedside, it is quick, and it is noninvasive. It poses no risk of radiation and is easily repeatable. However, it is operator dependent.53 Surgeons trained in FAST are more accurate in assessing the upper quadrants than in using the pericardial or pelvic view.54 Also, FAST does not reliably exclude intestinal injuries.3
The negative predictive value of FAST in children is not as high as in adults.5 In 26% to 35% of pediatric patients, there will be no evidence of hemoperitoneum on FAST but blood will be detected on CT scan.5,54 A negative FAST is not sufficient alone to exclude hemoperitoneum, but a positive FAST warrants further evaluation.3 If the FAST is positive and the patient is hemodynamically unstable, emergent transfer to the operating room is indicated.
In a study of 543 injured children, a positive FAST exam was confirmed on CT in 61/73 patients. A CT scan detected free fluid in 62/448 patients with a negative FAST, yielding a sensitivity of 50%, a specificity of 88%, a positive predictive value (PPV) of 84%, and a negative predictive value (NPV) of 58%. When the data were subgrouped, the examination was found to have lower sensitivity and specificity in children younger than 2 years old.53 One small study of 313 pediatric patients showed a 92.5% sensitivity and 97.2% specificity for detecting abdominal injury.55
Scaife et al asked surgeons the most common reason for ordering a CT scan when assessing a child who has sustained abdominal trauma.54 Their answers, in order of priority, were mechanism of injury, physical examination findings, and mental status. Surgeons at the authors’ institution received formal FAST training that then was integrated into their routine evaluation. After integration, they were asked if FAST results would change their mind about ordering CT scans. Normal findings on FAST and physical examination would have led the surgeons to cancel almost half of the CT scans. A positive FAST exam took one patient directly to the operating room. In 13 cases where the FAST was negative, the surgeon actually cancelled the CT scan. Fifteen percent of those patients for whom the CT was cancelled on the basis of the FAST had a falsely negative FAST exam.54
For patients in whom there is low suspicion of intra-abdominal injury, the use of the FAST exam has decreased the use of CT scans.52 The sensitivity of FAST can be improved by combining it with other tests (AST, ALT, and UA).6 Studies still need to be conducted in pediatrics regarding the efficacy of observing a patient for several hours after a negative FAST and the utility of repeating the exam. Repeating the FAST exam has not proven to be beneficial in adult patients.52 FAST can add information quickly and easily when evaluating a pediatric trauma patient. Although the exam is not perfect, the results can save time, can indicate whether the hemodynamically unstable patient should be taken to the operating room, and can spare patients with low suspicion for intra-abdominal injury from radiation when combined with the physical examination and laboratory values.
Computed Tomography
CT with intravenous contrast is the gold standard test for detecting intra-abdominal injuries in hemodynamically stable patients.3 Fifty percent of children who require a formal trauma evaluation will have an abdominal CT scan.54 The risk of subsequently detecting an intra-abdominal injury after a negative CT scan is 0.19%, giving a negative predictive value of 99.8%.3,56 Less than 15% of all abdominal CT scans done for concern for injury reveal an intra-abdominal injury.56 In 90% of patients, the CT scan does not influence the choice of treatment.57 Injuries that were missed on CT scan with IV contrast involved the intestines or pancreas.56
Oral contrast should be used if pancreatic or viscus injury is suspected.58 The administration of oral contrast may prove difficult in pediatric patients for reasons such as fear, pain, nausea, or change in mental status. The time to CT scan, especially in critically ill patients, might not be sufficient for the contrast to travel through the intestines. Oral contrast can remain in the stomach and interfere with other emergent studies, such as angiography. It also presents an aspiration risk. Ellison and colleagues found no significant differences in the sensitivity of CT scan with or without oral contrast with regard to detecting abdominal injury. The specificity when using oral contrast was slightly better.59 The risks and benefits of oral contrast should be considered prior to committing a patient to receiving it, especially since it does not increase sensitivity. Oral contrast should not be used if the patient cannot protect his or her airway.
The necessity for CT scans also has come under scrutiny because of radiation and its inherent risk of cancer. Each year, approximately 4,870 cancers can be traced to pediatric CT scans.60 The risk of future malignancy is based on age at exposure. A 1-year-old who has an abdominal CT scan has a 0.18% lifetime risk of cancer.61 The rate of cancer per single CT scan is 1 in 570-6,130 if the patient is younger than 10 years of age.62 The risk of solid organ cancer is 1 in 300-390 for girls and 1 in 670-760 for boys.63 The lifetime mortality rate from a single CT scan is 0.08%.64 Many protocols call for ALARA (as low as reasonably achievable) radiation doses, especially in children.64 CT scans of the abdomen deliver high doses of radiation to sensitive breast and colon tissue.60 Because of these considerations, a significant amount of effort has been directed toward safely reducing the number of CT scans ordered in the ED.
In 2013, Holmes et al evaluated several criteria that, when combined, are aimed at decreasing the number of abdominal CT scans. These criteria are: evidence of abdominal wall trauma, GCS score < 14, abdominal tenderness, evidence of thoracic wall trauma, complaints of abdominal pain, decreased breath sounds, and vomiting. If none of these criteria are met, the sensitivity is 97% for indicating no abdominal injury, with a negative predictive value of 99.9%, but a specificity of 42.5%. The children who were missed by these clinical criteria all had hemoperitoneum detected on FAST exam and distracting injury, intoxication, or abnormal laboratory findings. Children with none of these findings are at very low risk of having an abdominal injury that would require acute intervention.65 Lab testing along with FAST and observation instead of CT scan may be used in patients who meet one or none of the criteria.3
Another clinical prediction rule was developed via retrospective review by Acker and colleagues.62 Children who are 4 years of age and older are considered low risk if the injury is attributable to a single, non-motorized blunt force trauma, the GCS score is 15, and the pediatric adjusted shock index is normal. In this study, 101 of 206 patients were considered low risk. One patient in the low-risk group received a blood transfusion and none went to surgery. When the Holmes criteria were applied to this group, 14 of the 101 patients would have been observed. The probability of undergoing intervention in the low-risk group was < 1%.62
The Blunt Abdominal Trauma in Children (BATiC) allots points to ultrasound, abdominal pain, peritoneal irritation, hemodynamic instability, AST, ALT, WBC, lactate dehydrogenase, and lipase (or amylase). In a retrospective validation study performed by de Jong and associates, none of the patients with a BATiC score of 6 or less had intra-abdominal injury. If the BATiC system had been applied to the patients in this study group, the number of CT scans would have been reduced by 47%.57 Combining FAST with clinical decision rules may decrease the rate of abdominal CT.26
The rate of CT scanning increases as clinical suspicion increases. The study by Mahajon et al compared clinical suspicion with the clinical prediction rule. In this study, 35 children with clinical suspicion < 1% had an intra-abdominal injury requiring acute intervention; 3/25 of those children were low risk according to the clinical decision rules established by Holmes et al in 2013. Three percent of patients with acute intra-abdominal injury with acute intervention were not identified by the rule. The clinical prediction rule was more sensitive than clinical suspicion but less specific. Clinicians still ordered CT scans on one-third of patients whom they suspected of having < 1% risk of intra-abdominal injury; therefore, they did not practice based on their clinical suspicion. The reasons for ordering CT scans despite their clinical suspicion were mechanism of injury, abnormal abdominal exam, or request of the trauma team.63 Hynick found that undergoing a head CT scan was associated with getting a CT of the abdomen and pelvis.26 Providers need to be aware of these validated clinical decision rules and incorporate them into practice with the hope of reducing pediatric radiation exposure while not compromising patient care. Not all children involved in trauma need to have a CT scan of their entire body. Patient history, physical exam, laboratory findings, and clinical decision rules should be used to determine the necessity of each CT scan.
Many injured children are evaluated at a local hospital and then transferred to a tertiary pediatric center. As soon as a trauma patient is identified in the community setting, it is helpful to call the tertiary center so that transport can begin to be arranged as soon as possible. Imaging prior to transfer may not be needed. Eighty percent of pediatric trauma patients who are transferred to a Level I trauma center have a repeat CT scan.3 Up to 40% of abdominal CT scans are repeated.66 When possible, imaging decisions should be made in conjunction with a pediatric trauma center. Also, depending on local resources, a tertiary center may have the ability to produce smaller image slices, allowing for better quality. Patients who are transferred to a pediatric trauma center benefit from having their CT scan re-read by a pediatric radiologist. Onwubiko and Mooney compared outside hospital CT readings with a pediatric radiologist’s interpretation of the outside hospital’s film. Of 98 cases, 12 new injuries were identified, three solid organ injuries were upgraded in severity, and four patients were found not to have any injury. In this study, 19% of patients had a clinically significant change in their CT read.57 On transfer, CT scans should always be sent and, if possible, reinterpreted by a pediatric radiologist as opposed to reimaging the patient.
Diagnostic Peritoneal Lavage
Diagnostic peritoneal lavage (DPL) has fallen out of favor with the increased use of FAST and CT scanning in children. DPL is less specific than laparotomy, and it does not provide information about the retroperitoneum. DPL may lead to harmful side effects or unnecessary exploration.6 However, in resource-limited areas, DPL might be the only alternative to exploratory surgery.
Angiography
Data regarding embolization in pediatric patients is limited.3 Teens, those with closed head injury, and those treated at adult trauma centers are more likely to undergo embolization.67 Angiography has been used in only 3.2% to 4.1% of pediatric patients with blunt splenic trauma and should be used as an adjunct to nonoperative management.5,67,68 Nghia-Jack et al looked 97 pediatric patients over an 11-year period who underwent abdominal or pelvic angiography. The majority of these patients had high injury severity scores. Hemorrhage control was achieved in 87%. The mortality rate was 22%, with most deaths related to other catastrophic injuries.69 Risks of angiography, occurring in up to 7% of patients, include postembolization syndrome, hepatic abscesses, bile leak, and urinary incontinence.5,69
Contrast blush on CT scan can indicate active extravasation. Can patients with contrast blush be managed conservatively without angiography? Bansal et al looked at 270 pediatric patients with blunt splenic injury. Contrast blush was seen in 47 of them. There was no difference in the need for blood transfusion, length of stay, or splenectomy rates when children with contrast blush and no contrast blush were compared. Bansal argues that these children should be observed closely and their management should be based on hemodynamics and resuscitation over the appearance of contrast blush on CT scan.67
Contrast-Enhanced Ultrasound
As the FAST exam is gaining popularity and every effort is being made to decrease radiation exposure, another new technique has been developed. Contrast-enhanced ultrasound using microbubbles, similar to a bubble study on cardiac echocardiography, is being used widely in Europe as a follow-up study to blunt solid organ injuries. Microbubbles remain in the vascular space.3 Second-generation contrast agents such as perfluorocarbon and sulfur hexafluoride encapsulated in a phospholipid shell are stabilized gas microbubbles.70 They display nonlinear reverberation and remain fundamentally intravascular. These agents are approved by the U.S. Food and Drug Administration only for cardiovascular studies. They allow continuous depiction of the injury through arterial and venous flow. A trained sonographer needs about 10 minutes to assess an organ. The contrast is not yet licensed for use in lactating or pregnant women but is safe for children and renal patients. Studies in adults are promising.3
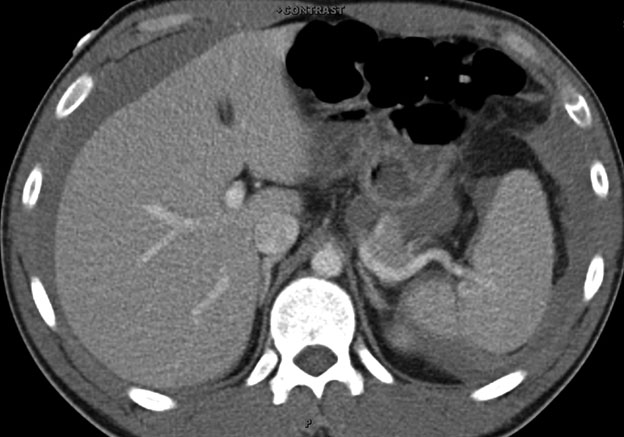
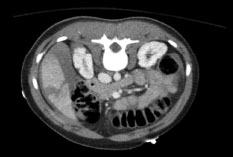
Contrast-enhanced ultrasound can reveal active bleeding and pseudoaneurysms in early stages of development and has been shown to outperform traditional ultrasound in the assessment of renal trauma.70 Some researchers have suggested that up to one-third of solid organ injuries can present without hemoperitoneum, so the injury would be missed on a standard FAST exam. In a retrospective review, all parenchymal bleeds were detected by contrast-enhanced ultrasound as well as CT scan. Traditional ultrasound missed 62% of the parenchymal lesions.71 (See Figures 2 and 3.) Contrast-enhanced ultrasound has the ability to decrease radiation exposure in the hemodynamically stable patient. Although contrast-enhanced ultrasound might not be used during initial resuscitation, it has many promising uses during reevaluation and in the future could become more widely studied and utilized.
Figure 2. Unremarkable Spleen in B-mode in 19 yo Trauma Patient

Reprinted from: Brader E, Halldorson C. Updates in pediatric trauma. Part I. Pediatr Emerg Med Rep 2015;20:40.
Figure 3. CT Scan of Patient Showing Fracture of Medial Aspect of Spleen Undetected on B-mode
Reprinted from: Brader E, Halldorson C. Updates in pediatric trauma. Part I. Pediatr Emerg Med Rep 2015;20:40.
Definitive Management
Most solid organ injuries can be managed nonoperatively.5 Low-grade liver or spleen injury rarely leads to clinically significant bleeding in children, perhaps because of their small blood vessels and enhanced vasoconstrictor response.9,62 Younger patients are more likely to require some type of intervention such as blood transfusion or surgery.36 The most common therapeutic intervention is blood transfusion.47,68
The Pediatric Emergency Care Applied Research Network (PECARN) collected data on 12,044 children with blunt abdominal trauma; 605 of them had solid organ injury. CT scan revealed fluid in 461, and 14 underwent laparotomy. The liver and spleen had the same rate of injury. With isolated organ injury, the liver was injured more than the spleen. Mechanisms of injury in this study group included fewer MVCs than in adults but higher rates of bike crashes and pedestrians being struck. The majority of patients in this study were managed without surgery.68
Patients who are hemodynamically unstable and do not respond to crystalloids or blood should be taken to the operating room. In another study, 119 of 16,321 pediatric trauma patients required abdominal exploration. Eighty-one underwent laparotomy and 38 had laparoscopic surgery. Seven laparoscopic patients required conversion to laparotomy.72 Laparoscopy might be preferred over laparotomy in a select group of patients. The organs injured and the hemodynamics of the patient ultimately dictate the disposition.
Splenic Injuries
The spleen is the most frequently injured abdominal organ, accounting for up to 45% of visceral injuries.3,6 In hemodynamically stable patients, routine management includes bed rest, serial hematocrit measurements, and serial physical examinations.3 The American Pediatric Surgical Association recommends nonoperative management for spleen and liver injuries of Grades 1 through 4.3,6 For severe injuries, patients need to be vaccinated for encapsulated organisms.3 In a study by Bansel et al, sports-related injuries were the most common cause of isolated splenic injury, followed by MVCs, falls, and then pedestrians struck. MVCs were the most common cause in polytrauma patients. Length of hospital stay was longer for patients with Grade 3 and 4 injuries. There is a higher success rate for nonoperative management in children than in adults. One hypothesis is that children have more myoepithelial cells, giving them more efficient contraction and retraction of the arterioles, and a thicker splenic capsule.67 Splenectomy rates are as low as 3% in children with isolated splenic trauma.73 Higher grade injuries are more likely to require operative intervention.68
Liver Injuries
The liver is the second most common organ injured in blunt abdominal trauma. An AST concentration > 200 U/L or an ALT level > 125 U/L (or either > 80 U/L after NAT) is indicative of liver injury.42 Nonoperative management is recommended in hemodynamically stable patients and for those who receive less than 40 mL/kg of blood. Arterial embolization has the same outcomes as conservative management. Complications of embolization specific to the liver include biloma, hepatic artery pseudoaneurysm, and necrotic gallbladder.3
Renal Trauma
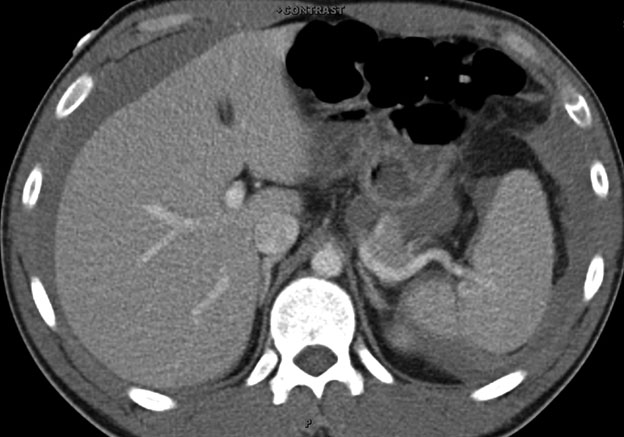
Renal trauma accounts for up to 10% of pediatric blunt abdominal trauma. It occurs more frequently in children than in adults. Associated injuries are found in 90% of cases.3 (See Figure 4.) CT is indicated if there is a significant mechanism of injury, flank bruising, thoracolumbar spine fracture, lower rib fracture, or gross hematuria.74 The management of microscopic hematuria is more controversial. The absence of hematuria does not rule out injury.44-46 Most blunt renal injuries are managed conservatively, with only 6.3% requiring operative intervention.66,73 The majority of renal trauma is low grade and is sustained by children older than 5 years of age. The rate of nephrectomy is higher for children treated at a trauma center that receives primarily adults compared with pediatric trauma centers. Penetrating trauma accounts for less than 10% of the injuries.75
Figure 4. CT Scan Showing Liver Laceration and Right Perinephric Hematoma
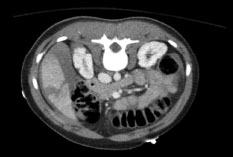
Image courtesy of Aaron Leetch, MD.
Acute kidney injury, indicated by an elevated creatine kinase level, occurred in 13% of the pediatric trauma patients in the study by Talving and colleagues.76 Independent risk factors included creatinine kinase concentration > 3000 IU/L, Injury Severity Score ≤ 15, GCS < 9, three or fewer imaging studies with contrast, blunt mechanism of injury, and fluid requirement in the emergency department.76 Patients who are at high risk of developing acute kidney injury need to have aggressive fluid resuscitation and serial measurements of kidney function.
The pancreas is the fourth most injured intra-abdominal organ, accounting for 2-9% of abdominal injuries.77 Blunt trauma squeezes the pancreas against the spine.5 Pancreatic injury in children might have a delayed presentation, even up to several weeks. Patients with pancreatic injury present with abdominal pain, nausea, vomiting, and fever. Complications include fistula formation, pancreatitis, and pseudocysts. Most cases can be managed nonoperatively with bowel rest, nasogastric tube placement, and parenteral nutrition. Ductal injury is a predictor of failure of conservative management.77
Pancreatic enzymes rise slower in children than in adults.3 Initial serum amylase and lipase values are not sensitive at detecting injury.24 The amylase concentration might be normal at first and should be reevaluated if suspicion of injury is high. The peak level of amylase is associated with the development of pancreatic pseudocysts. The lipase concentration also can be checked to exclude amylase originating from the salivary glands. Although lipase is considered more specific for the pancreas, many of the pediatric studies evaluating for pancreatic injuries have used amylase, and only occasionally lipase, as the main laboratory marker for pancreatic injury.78 A normal pancreas on the initial CT scan does not exclude pancreatic injury; the patient might require repeat CT scan, evaluation with ultrasound, or endoscopic retrograde cholangiopancreatography (ERCP). ERCP is the most utilized test when a CT scan is inconclusive.77
Hollow viscus injuries occur in 1-5% of children with abdominal trauma. The jejunum is injured in 30% of these cases and the duodenum in 2-10%. The colon is injured in 2-5% of pediatric cases of blunt trauma. Gastric perforations are rare.5 Intestinal injuries are caused by NAT, handlebar injuries, falls, and MVCs.79 CT has a high false-negative rate for perforation, especially when completed within the first several hours after trauma, so a high level of suspicion based on mechanism of injury is required.80 Unlike solid organ injuries, hollow viscus injuries often require surgical intervention.3 Peritonitis caused by bowel perforation takes time to develop, which can lead to a delay in presentation and diagnosis.80
Patients with duodenal hematomas can present after 24-48 hours with bilious vomiting.5,6 The hematoma can cause partial or complete small bowel obstruction, which normally can be managed conservatively.5,6,79 Hematomas typically develop in the second part of the duodenum.79
The inferior vena cava (IVC) is the most commonly injured intra-abdominal vessel in blunt abdominal trauma, with a 64% mortality rate among patients who present hemodynamically unstable. Seatbelt injuries are directly associated with IVC injuries. The hepatic vein also can be injured, which is typically fatal if hemodynamics are affected. Abdominal venous injuries have a 60% mortality rate overall (a three times greater risk of death compared with isolated arterial injuries).81 Abdominal aortic injuries are rare.6 Their leading cause is an MVC. Aortic injury also is associated highly with thoracic and pelvic injuries.82 Patients with vascular injury require operative management.81
Given the location of the adrenal glands and the protection afforded by other organs, they have a low incidence of injury. The incidence of adrenal injury is similar between adults and children who have sustained blunt abdominal trauma, ranging from 0.15% to 4.95%.83 CT is the best modality for visualizing these injuries. The mortality rate and injury severity are high when this particular injury is encountered, likely due to the force required to damage the gland and the subsequent endocrine deficiency. The right adrenal gland is injured more often than the left, possibly due to increased pressure in the inferior vena cava and compression between the liver and the spine. Patients with bilateral adrenal injuries typically are injured more severely than those with unilateral injuries. All patients with adrenal injuries should be monitored closely. These injuries induce no specific symptoms and commonly are discovered when imaging is performed. For most patients, care is supportive and revolves around the associated injuries. Steroid therapy may be considered for patients with bilateral injuries.83
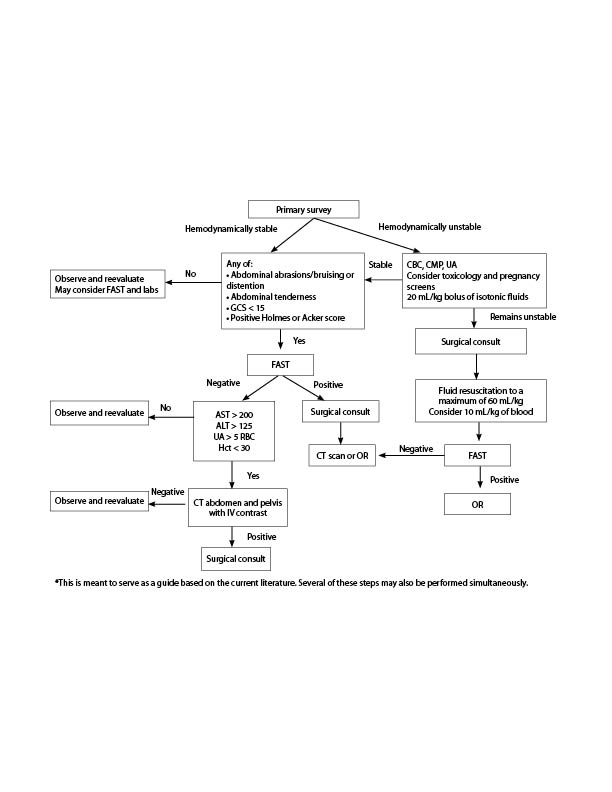
Pediatric trauma patients present challenges in the ED and can be anxiety provoking. Key information to obtain about a child suspected of having abdominal trauma includes the mechanism of injury, the treatment that was administered in the field, and the initial vital signs. Management of the patient should proceed similar to that for any trauma patient, with emphasis on fluid resuscitation, pain control, and the abdominal examination. Laboratory evaluation should include hematocrit, AST, ALT, and UA. FAST should be incorporated into the initial examination, because its findings can be very useful in conjunction with those of the physical exam and laboratory testing. (See Figure 5.) Clinical decision scores such as the one developed by Holmes et al or the BATiC score should be given significant weight in decisions regarding CT for a child with abdominal trauma. When the patient is hemodynamically stable, solid organ injuries can be managed mainly conservatively, but viscus perforations likely will require surgical intervention.