Common Orthopedic Injuries
February 15, 2017
Reprints
AUTHORS
Catherine A. Marco, MD, FACEP, Professor, Emergency Medicine and Surgery, Wright State University, Dayton, OH.
Ashley Humphries, MD, Wright State University, Dayton, OH.
Eric Mozeleski, MD, Wright State University, Dayton, OH.
PEER REVIEWER
Jonathan Glauser, MD, Professor, Case Western Reserve University, School of Medicine, Cleveland, OH.
Statement of Financial Disclosure
To reveal any potential bias in this publication, and in accordance with Accreditation Council for Continuing Medical Education guidelines, we disclose that Dr. Farel (CME question reviewer) owns stock in Johnson & Johnson. Dr. Schneider (editor), Dr. Stapczynski (editor), Ms. Fessler (nurse planner), Dr. Marco (author), Dr. Humphries (author), Dr. Mozeleski (author), Dr. Glauser (peer reviewer), Ms. Mark (executive editor), Ms. Coplin (executive editor), and Ms. Hatcher (managing editor) report no financial relationships with companies related to the field of study covered by this CME activity.
EXECUTIVE SUMMARY
- Vascular insufficiency or injury with extremity trauma is a true emergency. If there is joint deformity associated, immediate fracture reduction should be attempted.
- A fall on an outstretched arm causes different injuries at different ages. In the young, it may cause supracondylar fractures of the elbow, and in the elderly, it may cause a distal radial fracture.
- Navicular fractures often are hard to see on X-ray. Tenderness at the snuffbox with a history of a fall should lead to immobiliztion, in most cases with orthopedic follow-up.
- There are a number of methods proven to reduce a shoulder dislocation. If one does not work, a second or third technique should be tried.
Approach to Orthopedic Injuries
Orthopedic injuries are a common reason for emergency department (ED) visits. Orthopedic injuries should be diagnosed promptly and accurately and treated to optimize the outcome. Orthopedic injuries may be associated with chronic disability or pain. Patients with the following risk factors may be at higher risk for chronic pain following injury: female gender, older age, preinjury anxiety or depression, fewer years of education, and high pain intensity.1 The number of comorbid conditions has been associated with disability following injury.2
The initial ED evaluation should consist of assessment and stabilization of airway, breathing, and circulation. Assessment of neurovascular status of the injury is a priority. If there is evidence of compromised circulation, immediate reduction of the fracture or dislocation is indicated. If neurovascular status is intact, the ED evaluation should continue and should consist of a history, including mechanism of injury and associated injuries, and physical examination, with focused attention on appearance, vascular status (including pulses and capillary refill), range of motion, area(s) of tenderness or deformity, and neurologic status, including sensation and function. Jewelry should be removed. Tetanus immunization is given if appropriate, and antibiotics started for an open fracture. If a fracture or foreign body is suspected, radiographs are indicated. (See Figure 1.)
Figure 1. Approach to Orthopedic Injuries
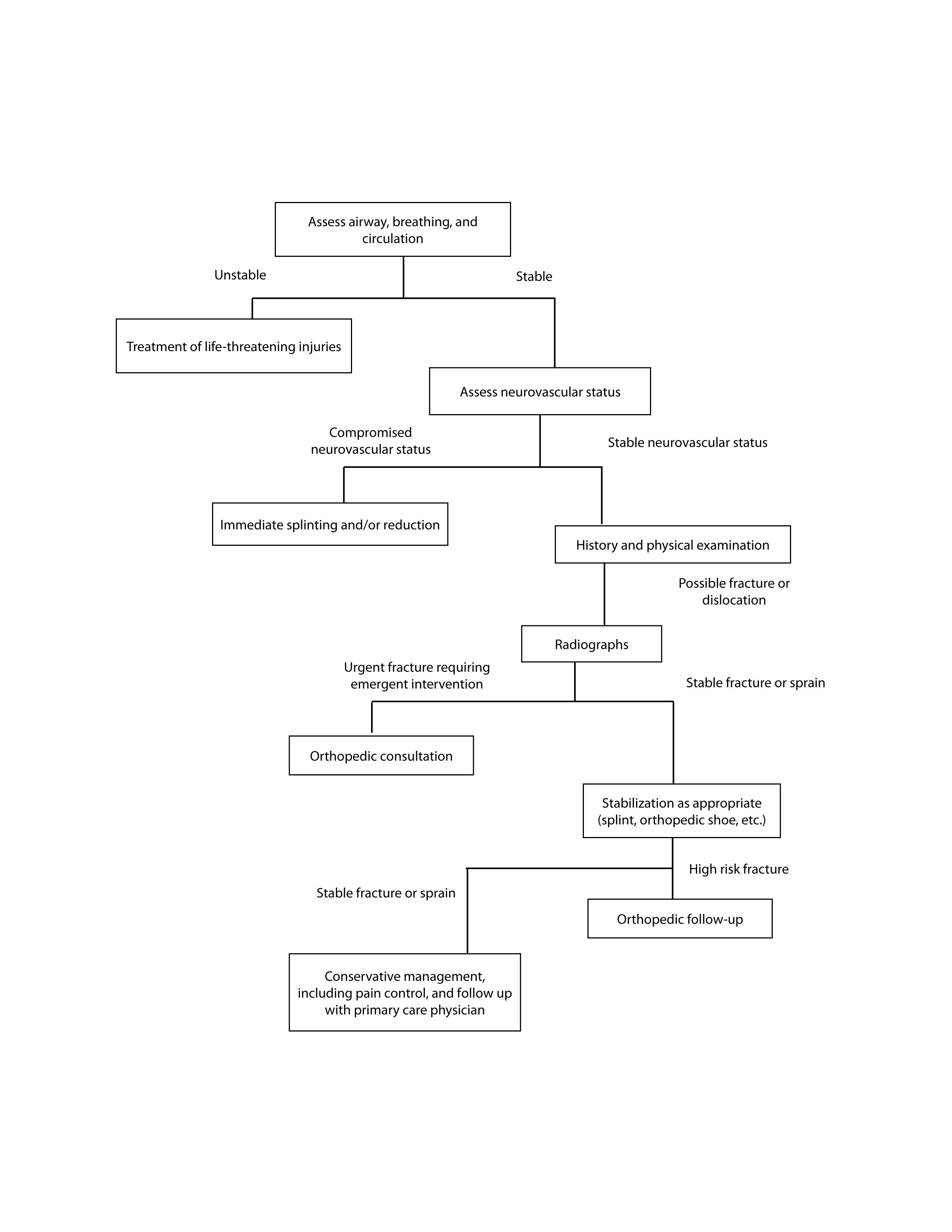
Sprains and strains are common among ED patients with extremity trauma. After a fracture is ruled out, the joint should be immobilized and the patient should be treated with pain control and outpatient follow-up. Early mobilization is important to improve outcomes. Physical therapy may be indicated in some cases.
Fractures should be identified and treated in the ED. Types of fractures include common fractures, pathologic fractures, stress fractures, and epiphyseal plate fractures.3 Orthopedic injuries requiring emergent intervention include open fractures, dislocations, and those causing neurovascular compromise.
Radiographs often are indicated to diagnose possible fractures. Generally, it is recommended that the joint above and below the injury also be examined by radiography because of the potential of referred pain. Some nondisplaced fractures may not be identified on the day of injury. For suspected fractures without radiographic evidence, the extremity should be immobilized, with repeat radiographs in 7-10 days. Clinically, if there is still concern for a fracture (severe pain, inability to bear weight), CT or MRI should be considered.
Pain control may include pharmacologic management with oral acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs) for patients younger than age 65 years with normal renal function, or opioid analgesia.4 Regional anesthesia may be preferred, particularly for distal radius (hematoma block) or hip fractures (femoral nerve block).
This article reviews several common orthopedic injuries, with specific focus on the appropriate ED evaluation and management.
Distal Radius Fractures
Wrist injuries are common ED complaints.5 The distal radius is the most commonly fractured bone of the wrist, and accounts for 20% of fractures in patients older than age 65 years.6 A fall on an outstretched arm is a common mechanism of injury. Patient age often is a determining factor for the injured structure after such a fall. Pediatric patients typically injure the metaphysis or epiphyseal plate of the radius, or sustain a supracondylar fracture of the humerus. Adults injure the navicular bone or wrist ligaments. Older adults may injure the distal radius.
Patients with a distal radial fracture present with pain and swelling. A physical examination typically reveals swelling and deformity of the distal radius. A “dinner fork” deformity of the wrist may be seen with a Colles’ fracture.
Imaging of the wrist should include four views. Distal radius fractures typically are evident on plain radiographs and rarely require additional imaging.
A Colles’ fracture is a fracture of the distal radius with dorsal angulation and proximal and dorsal displacement. (See Figures 2 A and B.) Angulation of greater than 20 degrees is considered unstable and may be associated with increased risk of distal joint instability and resultant arthritis.
Figure 2A. Distal Radius Fracture, AP View

Figure 2B. Distal Radius Fracture, Lateral View

Pain control is essential and may include parenteral opioid therapy, intravenous regional anesthesia, regional nerve block, or hematoma block.7
For stable fractures with less than 20 degrees angulation, ED management includes pain control, splinting, and follow-up with an orthopedic surgeon. For fractures with significant angulation, closed reduction can be performed in the ED. A hematoma block generally achieves adequate analgesia, with injection of 5-10 cc of 1% lidocaine through the dorsal forearm into the fracture space.8,9 The deformity then is reduced with elongation of the fracture using finger traps and traction with weight at the elbow. A sugar tong splint is applied to provide immobilization.
Open fractures or fractures with neurovascular compromise indicate the need for emergent orthopedic consultation. Fractures with severe comminution, intraarticular involvement, or those that are unstable should be referred for orthopedic consultation for possible surgical repair. Complications of Colles’ fracture may include malunion, joint instability, arthritis, or median nerve injury.
A Smith’s fracture (or reverse Colles’ fracture) is a fracture of the distal radius with volar displacement. As with Colles’ fractures, Smith’s fractures are treated with pain control, immobilization, and closed reduction for significant displacement.
Shoulder Dislocation
Shoulder dislocation is an orthopedic emergency. It is estimated that approximately 50% of joint dislocations are shoulder dislocations.10 Shoulder dislocations are common because of the instability of the shoulder joint. The glenoid fossa is very shallow, providing a large range of motion but a small amount of support, causing the joint to be very unstable. The four rotator cuff muscles provide a large amount of support for the joint. The axillary nerve wraps around the neck of the humerus and is the most commonly injured nerve in shoulder injuries. It is more common in the younger male population and the older female population.
Anterior shoulder dislocations account for 95% or more of shoulder dislocations. In patients younger than 40 years of age, it is estimated that close to half will undergo shoulder surgery due to complications post-reduction.11
The most common mechanism causing anterior shoulder dislocations is forced abduction and external rotation. Commonly, this is seen in sports such as basketball and volleyball when a block is being performed with an extended arm. In the elderly it can be seen following a fall on an outstretched hand (FOOSH).
The differential diagnosis includes humeral head fracture, posterior shoulder dislocation, inferior shoulder dislocation, acromioclavicular separation, and rotator cuff injury.
On physical exam, the patient’s normal shoulder contour will appear flattened when compared with the non-dislocated shoulder. The acromion will be very prominent, representing the empty glenoid fossa. The patient will have pain on attempts at active or passive movement of the affected shoulder. Axillary nerve injury may be seen in 42% of patients with anterior shoulder dislocation, and usually resolves after reduction.12
Imaging is not mandatory prior to reduction, given the typical history and physical examination, without suspicion of fracture. If the physician is uncertain, he or she should obtain shoulder radiographs, including including an anteroposterior (AP) view, a scapular Y view, and an axillary view. Pre-reduction films help to confirm the dislocation and to rule out any fractures that may complicate the reduction. Concomitant fracture occurs in approximately 25% of cases.13 Post-reduction films help to confirm the reduction and to verify that no iatrogenic injury was caused by the reduction.
CT and MRI should be considered if there is concern for a fracture that is not well visualized on X-ray for neurovascular injury. A CT angiogram should be performed if there are any signs of vascular injuries.
There are three commonly associated fractures that coincide with anterior shoulder dislocation. First is the Hill-Sachs deformity, which is a depression in the humeral head caused by the glenoid rim during dislocation. Second is a Bankart lesion in which part of the anterior glenoid lip is avulsed. Third, fractures of the greater tuberositiy may occur due to shoulder dislocation/relocation.
Anterior shoulder dislocations should be reduced as soon as possible to minimize any neurovascular and bony damage. However, as with any situation, a more emergent or life- or limb-threatening issue will take precedence.
Immediate surgical management is necessary if there is neurovascular injury from fractures.
There are several different techniques to reduce an anteriorly displaced shoulder injury. There is no evidence to support a single approach as the best for all clinical scenarios. Often, if one approach is unsuccessful, another approach may be successful for that individual patient.
The external rotation technique is simple and has a success rate of 80-90%.14,15 It can be performed by a solo practitioner and requires no additional assistance. It is performed by having the patient lie supine with the elbow flexed at 90 degrees and shoulder adducted. The forearm then is rotated outward with supination. Some patients may need pain control, sedation, or intra-articular anesthetic to accomplish the procedure.
Other reduction techniques have been reported with variable success.16,17 Some common reduction methods include the Kocher maneuver (elbow flexed at 90 degrees, external rotation of the arm, then medial rotation), the Stimson method (the patient is prone with a weight attached to the affected wrist hanging off the stretcher), the Hippocratic method (traction along the axis of the arm with traction-countertraction), the Milch method (supine with slow abduction and external rotation of the arm to the overhead position, with traction on the extended elbow), and scapular manipulation (medial rotation of the inferior tip of the scapula while an assistant provides traction on the affected limb).
With a primary anterior dislocation, the likelihood of recurrence is high, and outpatient surgical attention may be required to fix rotator injuries and increase stabilization. Patients should have immobilization with a sling and swathe post-reduction and should be referred to orthopedics within one week. Usually, patients will remain in immobilization for about three weeks.
Navicular Fractures
The navicular (scaphoid) is the most commonly fractured carpal bone of the wrist. Pines and Everett report that navicular fractures represent 70-80% of all carpal bone fractures.18 The navicular is a boat-shaped carpal bone and is present in the anatomic snuff box of the wrist. The ulnar or medial border of the snuff box consists of the tendon of extensor pollicis longus. The radial or lateral border is made by the tendons of the abductor pollicis longus and extensor pollicis brevis. The proximal border is the styloid process of the radius. The navicular is divided into three sections: proximal pole, waist, and distal pole. The tubercle of the navicular is located on the distal pole. Most of the navicular is covered by articular cartilage, with only two small portions of the bone accessible by blood vessels. These portions include the proximal pole as well as a small part of the neck of the navicular. The major blood supply is the dorsal carpal branch of the radial artery. This branch enters the navicular on the dorsal surface and supplies 80% of the navicular via retrograde blood flow. Twenty percent of the navicular is supplied by the superficial palmar arch, a branch of the volar radial artery. This branch enters at the tubercle. Because of the tenuous nature of the blood supply and retrograde flow pattern, there is a high risk of non-union and avascular necrosis in undiagnosed and undertreated navicular fractures. Avascular necrosis most commonly forms in the proximal pole and eventually can lead to disabling arthritis.
Because the navicular lies in both rows of carpal bones, it tends to have less movement than the other carpals. The navicular acts as a bony block to extension at the wrist and frequently is fractured when an axial load is placed across an outstretched hand, otherwise known as a FOOSH injury. Injuries to the navicular occur frequently in contact sports and in patients susceptible to falling, such as the elderly, intoxicated individuals, and those ambulating during icy conditions. Navicular fractures are rare in children because the carpals are composed of cartilage until late childhood into early adolescence. In a 2010 study by Van Tassel et al, the incidence of navicular fracture was estimated at one out of 100,000 people per year.19 Injuries to the navicular can account for 15% of acute wrist injuries. Sixty-five percent of fractures of the navicular occur at the waist portion of the bone. Fracture to the proximal pole of the bone is estimated at 16-28%, with the remaining 10% occurring at the distal pole. A navicular fracture also may have an associated injury in 12% of cases, including injuries to the radius or other carpal bones, as well as dislocations and instability patterns.
Clinical presentation of patients typically consists of complaints of pain and swelling on the dorsal aspect of the wrist usually located just distal to the radial styloid process. As mentioned previously, this is the location of the anatomic snuff box. Pain also may be elicited with resisted pronation and palpation of the navicular tubercle on the palmar aspect of the wrist. Navicular fracture is unlikely without pain on examination in these two areas. Duckworth et al report that sensitivity for identifying fracture on clinical exam tends to be high; however, specificity can range from 74-80%.20
Diagnosing navicular fractures with radiographic imaging sometimes can be difficult with just AP and lateral views. Therefore, a special navicular view of the wrist should be ordered when clinical suspicion is high. This view is taken in 30 degrees of wrist extension with 20 degrees of ulnar deviation. According to Gerrman and Perron, it is estimated that 10-14% of navicular fractures are missed with plain imaging soon after injury occurs.21 Therefore, if imaging is negative and there remains a high index of suspicion, imaging should be repeated in two to three weeks along with referral to orthopedics. Hodgkinson et al describe a “scaphoid fat pad sign” in which there is soft tissue swelling with displacement of adjacent fat pads.22 Currently, MRI is the gold standard for detecting occult fractures with a sensitivity of 100%. Bone scan performed within 72 hours of injury traditionally was the test of choice for diagnosing occult fractures and also has been shown to have a high correlation with MRI in navicular injuries.
It is worth repeating that because of the high incidence of nonunion and avascular necrosis, immediate immobilization and referral to an orthopedic specialist is vital. Nonunion rates increase with delayed immobilization. According to Davenport, the more proximal, oblique, or displaced a fracture, the greater the risk of developing avascular necrosis. Oblique, rotated, comminuted, or fractures displaced greater than 1 mm are all considered unstable and require urgent surgical referral. Nonoperative management using thumb spica casting or splinting is indicated for stable nondisplaced fractures as well as for those injuries highly suspected for fracture. Duration of immobilization will be determined by the specialist and by location of the fracture. Fractures to the proximal pole may take up to five months to heal.
Hip Fractures
Hip pain represents a significant portion of ED visits. The complaint is highest among females age 65 years and older, representing 1.6% of ED visits in this population.24 Significant morbidity and mortality may result following hip fractures, and mortality may be as high as 38% at 24 months.25 Morbidity and mortality may be due to immobilization resulting in thromboembolism, infection, avascular necrosis, or decreased functional capacity. Advanced age, male gender, ASA classification, and significant comorbidities contribute to increased risk of mortality.26,27,28
Initial ED Management
Initial management should include assessment and stabilization of airway, breathing, and circulation. A history should be obtained, including any history of fall, syncope, or other trauma, as well as the location of pain. Pain from a hip fracture may be referred to the pelvis, knee, or leg.
Physical examination should include examination of the injured extremity, including resting position, ecchymosis, lacerations, deformity, neurovascular status, location of pain and tenderness, and a thorough examination to identify any additional injuries. Hip fractures often present with a foreshortened and externally rotated extremity, but these findings are not universal.
Pain control is essential. Pharma-cologic pain management may include treatment with opioids, an intravenous nonsteroidal drug, or acetaminophen. Regional nerve blocks may provide effective pain control and reduce the need for opioid therapy.29,30
Imaging should be obtained for all patients with possible hip fracture. Images of the hip and pelvis are indicated. Often, if the injury is radiographically subtle, a comparison view of the unaffected hip is helpful. CT or MRI may be considered for suspected fractures not identified on radiographs or to further classify the detailed anatomy of the injury.31
Classification of Hip Fractures
Hip fractures may be classified as intracapsular (including the femoral head and femoral neck) or extracapsular (including trochanteric fractures, intertrochanteric, and subtrochanteric). (See Figure 3.)
Figure 3. Classification of Hip Fractures
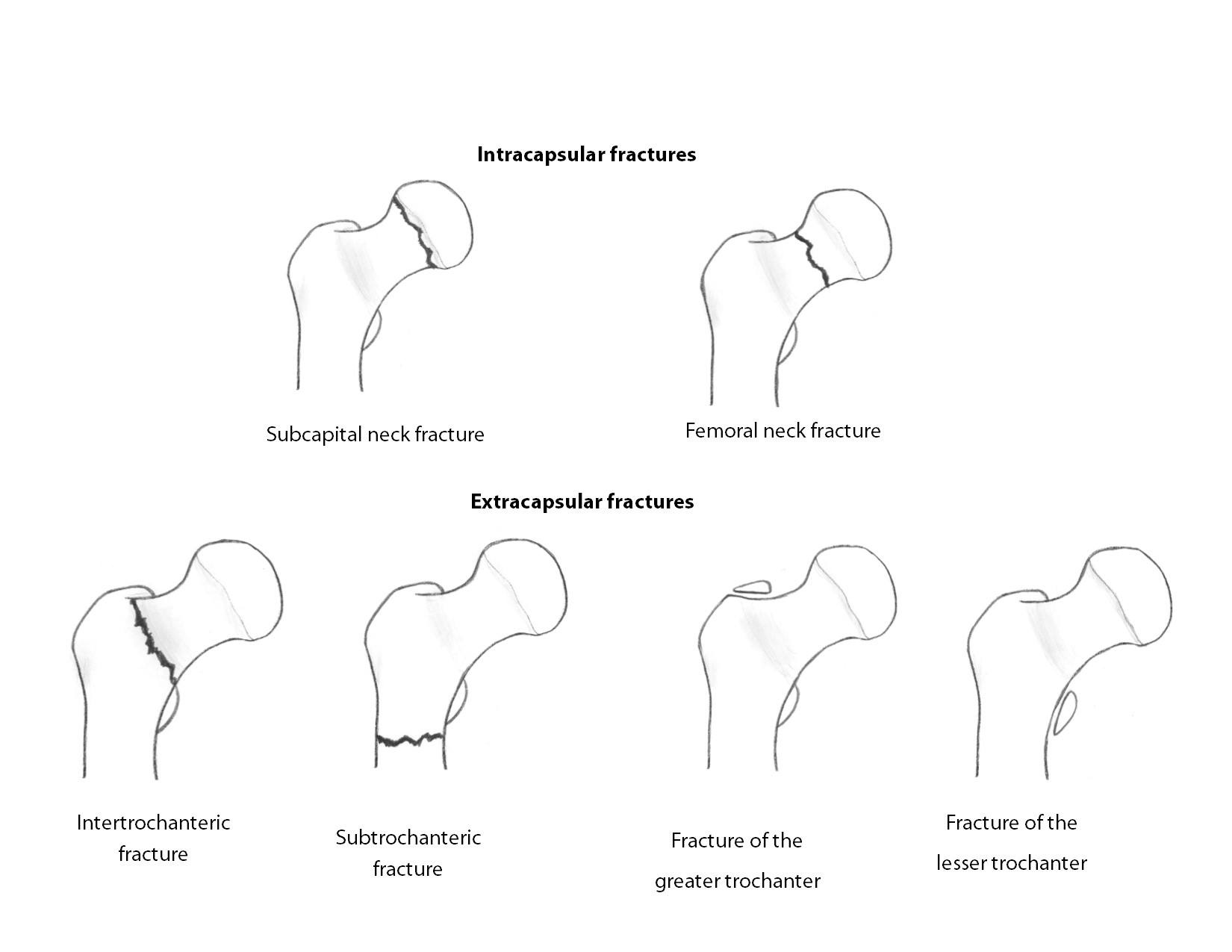
Intracapsular Hip Fractures
Femoral neck fractures commonly occur after falls in elderly patients with osteoporosis. Patients may present with minor or severe pain in the hip, leg, or groin. Patients with nondisplaced fractures may be ambulatory prior to ED arrival. Imaging should include AP and lateral views of the hip and pelvis. Radiographic findings may include a fracture line, altered neck-shaft angle (normally 120-130 degrees), or disruption of Shenton’s line (a curved line from the superior border or the obturator foramen to the medial aspect of the femoral metaphysis). (See Figure 4.) The AP view of the pelvis may be helpful is providing comparison views of the contralateral normal hip. The blood supply to the femoral head may be disrupted. Prompt treatment with immobilization and orthopedic consultation for definitive management is essential to providing the best possible outcome. Traction is not indicated for femoral neck fractures, as traction may further compromise blood supply to the femoral head. Complications may include avascular necrosis, infection, deep venous thrombosis, or pulmonary embolism.
Figure 4. Femoral Neck Fracture

Femoral head fractures are less common and often present with concurrent dislocation. If dislocation is present, emergent closed reduction should be performed. Immediate orthopedic consultation for definitive management is indicated. Potential future complications include avascular necrosis, sciatic nerve injury, heterotopic ossification, arthritis, infection, deep venous thrombosis, or pulmonary embolism.
Extracapsular Hip Fractures
Intertrochanteric Fractures. Intertrochanteric fractures are most common in elderly patients with osteoporosis or osteopenia as a result of direct trauma, most commonly falls.(See Figure 5A and B.) Patients typically present with severe pain, and the affected leg may be foreshortened and externally rotated. Prompt orthopedic consultation for definitive management is essential. Complications may include infection, deep venous thrombosis, or pulmonary embolism. Avascular necrosis or malunion are less common complications.
Figure 5A. Intertrochanteric Hip Fracture
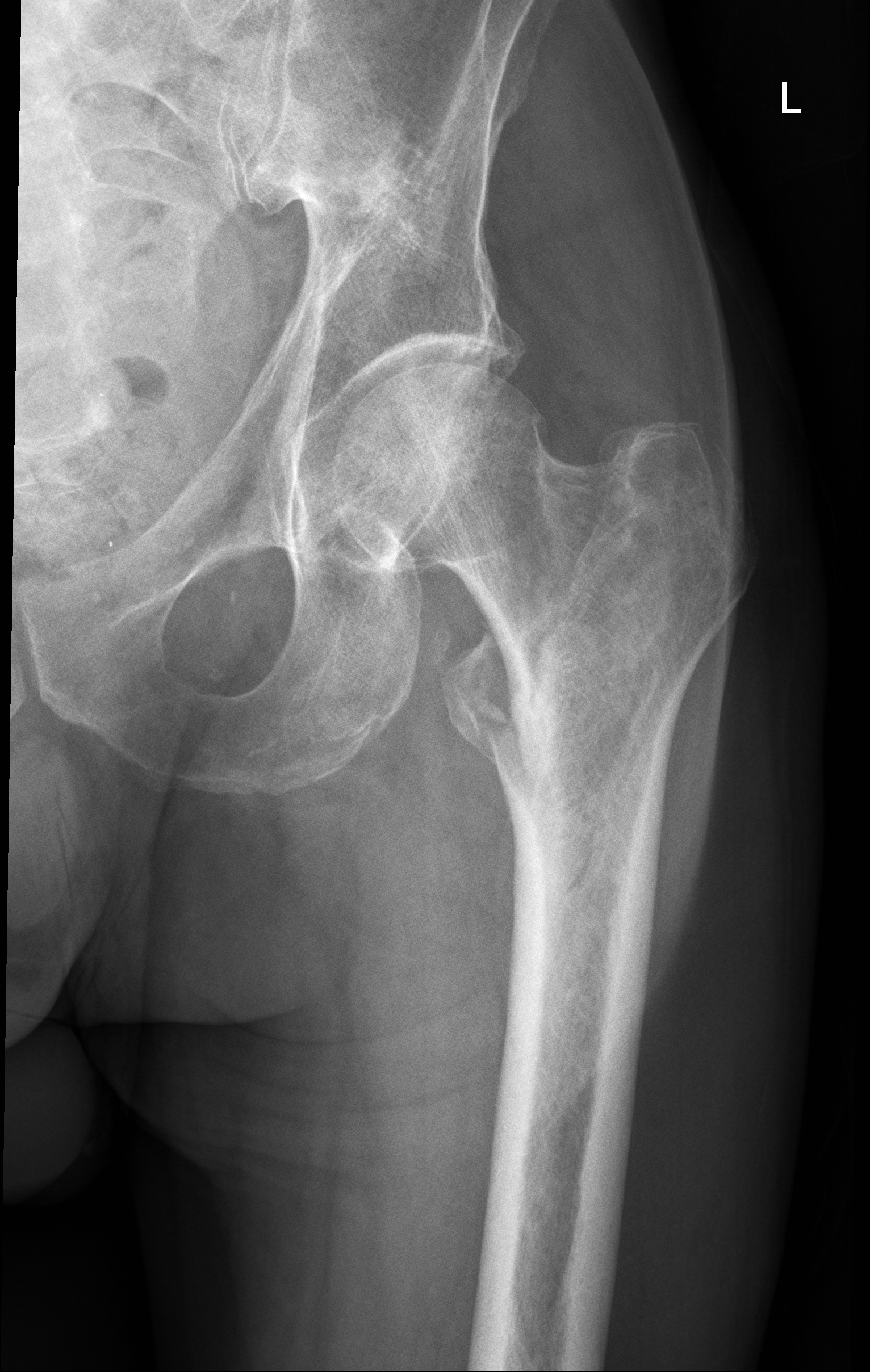
Figure 5B. Intertrochanteric Hip Fracture, Pelvis View

Trochanteric Fractures. Trochanteric fractures are less common. Fractures of the greater trochanter may result from direct trauma, or may result from an avulsion due to contraction of the gluteus medius, particularly in adolescent patients. Fractures of the lesser trochanter occur most commonly in adolescents, due to forceful contraction of the iliopsoas muscle.
Trochanteric fractures should be treated with conservative management including pain control and protected weightbearing. Open reduction with internal fixation may be indicated if there is more than 1 cm of displacement.
Subtrochanteric Fractures. Subtrochanteric fractures are common in the elderly population with osteoporosis or osteopenia, as a result of direct trauma, most commonly falls. Patients typically present with severe pain, and the affected leg may be foreshortened, abducted, and externally rotated. Prompt orthopedic consultation for definitive management is essential. Complications may include avascular necrosis, infection, deep venous thrombosis, or pulmonary embolism.
Prompt orthopedic consultation should be obtained for definitive management. Traction may be indicated. Devices may include Hare® (Dynamed, Westbury, Tasmania) or Sager® (Minto Research and Development, Inc., Redding, CA) splints. Complications may include avascular necrosis, malunion, nonunion, infection, deep venous thrombosis, or pulmonary embolism.
Definitive Management
Care of the patient with a hip fracture should be coordinated between the emergency physician, orthopedic surgeon, anesthesiologist, and geriatrician or primary care physician, if possible.32 In addition to surgical repair, medical management of nutritional status, pain control, hydration, electrolyte balance, rehabilitation, and fall prevention are essential to optimizing patient outcomes.33,34 The patient should be admitted for inpatient coordinated definitive management. Operative intervention within 48 hours is associated with improved outcomes, including independent living, reduced mortality, and reduced rates of infection.35
Ankle Sprains
Ankle sprains are common injuries seen in the ED. Ankle sprains may be classified as low ankle, including lateral ankle sprains and medial ankle sprains. High ankle (syndesmotic) sprains can also occur. Ankle sprains can range from stretching of the ligaments to partial or complete ligamentous rupture. Socioeconomic impact is high because of the prevalence and chronicity of this injury.36 Long-term complications, including re-injury, chronic ankle instability, and continued pain, are prevalent. Repeat ankle injuries are very common.
Patients will present following a twisting motion of the ankle joint (inversion or eversion). Physical examination may reveal swelling, ecchymosis, tenderness, pain with weight-bearing, and limited range of motion. Bony tenderness and ligamentous stability should be assessed. Syndesmosis injuries may have few physical examination findings.
Imaging is indicated to rule out a fracture. The Ottawa Ankle Rules for Ankle and Midfoot Injuries may be used to identify patients who should undergo imaging for possible fracture.37,38,39 (See Table 1.) Standard three view ankle series is recommended. CT and CT angiography (CTA) can be performed if there is a concern for vascular injury or skeletal injury not well visualized on radiographs. MRI can be considered in the outpatient setting for further management if the patient continues to have pain six to eight weeks later.
Table 1. Ottawa Ankle Rules for Ankle and Midfoot Injuries
Ankle imaging is indicated for:
- Malleolar pain
Plus one of the following:
- Bony tenderness of lateral malleolus
- Bony tenderness of medial malleolus
- Inability to bear weight immediately after injury and in the ED
Ankle sprains are graded from 1 to 3 depending on severity. A grade 1 is a stretching of the ligaments with only mild swelling, no joint instability, and tenderness. A grade 2 sprain involves an incomplete tear of a ligament. This will cause more swelling and ecchymosis as well as tenderness. The patient will be able to bear weight but will have painful ambulation. A grade 3 sprain includes a complete tear of a ligament. The patient will not be able to bear weight, and there will be instability on exam.
Treatment should include pain control and ankle support. Pain control is often recommended with NSAIDs, although evidence is limited to suggest their superiority in outcomes relative to other agents.40 Crutches can be given to patients who are unable to bear weight. Early mobilization is recommended.41,42,43 An ankle brace, such as Aircast, or ankle splint is associated with better outcomes as compared to a simple ACE wrap.44
Patients should be referred to an orthopedic surgeon if there is a neurovascular injury, dislocation, tendon rupture, or open fracture.
Patellar Dislocations
Patellar dislocations are an infrequent knee injury, accounting for approximately 3% of all knee injuries.45 The patella can dislocate superiorly, inferiorly, or laterally. The focus of this section will be on the laterally displaced patellar dislocations. The most common population to have acute patellar dislocations is the active and young population, contrary to the previous belief that the overweight and sedentary were most at risk.46 Elderly females may have chronic instability.47 There are several predisposing conditions that increase the likelihood of patellar dislocation including generalized joint laxity, iliotibial band tightness, previous patellar subluxation, and weakness of the vastus medialis muscle. Patients younger than the age of 15 years with patellar dislocations are more likely to have a recurrence.48
Patients often present after a twisting motion of their knee or a direct blow to the knee. This motion is seen in sports such as gymnastics, baseball, and dance. Usually this is described during physical activity. There is a natural force that pulls the patella laterally from the knee extensors; during flexion, this force is greatly increased, causing an increased likelihood of the patella to displace.50 Patients present with pain in the knee with visible deformity to the knee and swelling. The patient will hold the knee in a flexed position. Also, the patient likely will present with a hemarthrosis and have tenderness to the medial edge of the patella. Patients may describe the incident as “my knee gave out” and complain of pain.
The physical exam will show a lateral displacement of the patella with the knee joint held in flexion (usually 20-30 degrees).
The differential diagnosis includes patellar subluxation, patellar fracture, knee dislocation, fracture of femur, tibia, and fibula, ligamentous injury, or nerve or vascular injury.
Post-reduction knee films including AP, lateral, and “sunrise” views should be obtained to rule out fracture or avulsion. Forty percent of patients with a patellar dislocation also will have associated fractures. Pre-reduction films are not indicated, as they do not affect the success of the reduction.
Treatment is urgent to reduce the incidence of chronic pain, recurrent dislocations, or nerve or vascular compromise. Pain control with opioid analgesia is indicated. The patient should be placed supine with the affected hip flexed. The patella should be relocated by pushing the patella medially while extending the knee joint. Success is confirmed by the patient being able to flex and extend the affected knee joint. The patient then should be placed in a patellar stabilizing brace or knee immobilizer and given crutches for initial immobilization, with encouragement to bear weight as tolerated for three to four weeks.51 NSAIDs should be the primary outpatient pain medicine. Rest, ice, compression, and elevation should be encouraged. Patients will need outpatient follow-up with a possible MRI to look for ligamentous, cartilaginous, and soft tissue damage that may need further surgical workup. Patients who need orthopedic follow-up include those with recurrent dislocations, dislocation with fracture, children younger than 15 years of age, or dislocation coinciding with medial collateral ligament and/or anterior cruciate ligament injury. Patients should participate in rehabilitation with emphasis on quadriceps strengthening.
Pearls and Pitfalls
- Assessment of neurovascular status of the injury is essential. Injuries with associated vascular compromise should be reduced immediately.
- Pain control is essential. This may include pharmacologic therapy, immobilization, reduction, or regional anesthesia.
- Closed reduction should be performed for distal radius fractures with more than 20 degrees of angulation.
- Intracapsular hip fractures may be associated with impaired blood supply. Traction should not be used.
- Suspected navicular fractures should be immobilized and referred for orthopedic follow-up, even if imaging does not depict a fracture.
- Ankle sprains should be treated with NSAIDs, an ankle brace, and early immobilization.
- Shoulder dislocations should be reduced using the external rotation technique, scapular manipulation, or another reduction technique. Early reduction is essential.
REFERENCES
- Clay FJ, Watson WL, Newstead SV, McClure RJ. A systematic review of early prognostic factors for persistent pain following acute orthopedic trauma. Pain Res Manag 2012;17:5-44.
- Gabbe BJ, Harrison JE, Lyons RA, et al. Comparison of measures of comorbidity for predicting disability 12-months post-injury. BMC Health Serv Res 2013;13:30.
- Menkes JS. Initial evaluation and management of orthopedic injuries. In: Tintinalli JE, Stapczynski J, Ma O, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016.
- National Clinical Guideline Centre (UK). Fractures (Non-Complex): Assessment and Management. London: National Institute for Health and Care Excellence (UK); 2016 Feb. National Institute for Health and Care Excellence: Clinical Guidelines.
- Perron AD, Brady WJ. Evaluation and management of high-risk orthopedic emergency. Emerg Med Clin North Am 2003;21:159.
- Ikpeze TC, Smith HC, Lee DJ, Elfar JC. Distal radius fracture outcomes and rehabilitation. Geriatr Orthop Surg Rehabil 2016;7:202-205.
- Handoll HH, Madhok R, Dodds C. Anaesthesia for treating distal radial fracture in adults. Cochrane Database Syst Rev 2002;(3):CD003320.
- Myderrizi N, Mema B. The hematoma block an effective alternative for fracture reduction in distal radius fractures. Med Arh 2011;65:239-242.
- Padegimas EM, Ilyas AM. Distal radius fractures: Emergency department evaluation and management. Orthop Clin North Am 2015;46:259-270.
- Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am 2010;92:542.
- Hovelius L, Rahme H. Primary anterior dislocation of the shoulder: Long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc 2016;24:330-342.
- Visser CP, Coene LN, Brand R, Tavy DL. The incidence of nerve injury in anterior dislocation of the shoulder and its influence on functional recovery. A prospective clinical and EMG study. J Bone Joint Surg Br 1999;81:679.
- Perron AD, Ingerski MS, Brady WJ, et al. Acute complications associated with shoulder dislocation at an academic emergency department. J Emerg Med 2003;24:141.
- Eachempati KK, Dua A, Malhotra R, et al. The external rotation method for reduction of acute anterior dislocations and fracture-dislocations of the shoulder. J Bone Joint Surg Am 2004;86-A:2431.
- Janitzky AA, Akyol C, Kesapli M, et al. Anterior shoulder dislocations in busy emergency departments: The external rotation without sedation and analgesia (ERWOSA) method may be the first choice for reduction. Medicine (Baltimore) 2015;94:e1852.
- Khiami F, Gérometta A, Loriaut P. Management of recent first-time anterior shoulder dislocations. Orthop Traumatol Surg Res 2015;101(1 Suppl):S51-S57.
- Mallia AK, Milligan BT. Reduction of shoulder technique. Medscape, Sept. 2, 2016. Available at: http://emedicine.medscape.com/article/109130-technique#c3. Accessed Jan. 25, 2017.
- Pines JM, Everett WW. Evidence-Based Emergency Care, Diagnostic Testing and Clinical Decision Rules. BMJ Books; London; 2011.
- Van Tassel DC, Owens BD, Wolf JM. Incidence estimates and demographics of scaphoid fracture in the U.S. population.
J Hand Surg Am 2010;35:1242-1245. - Duckworth AD, Ring D, McQueen MM. Assessment of the suspected fracture of the scaphoid. J Bone Joint Surg Br 2011;93:713-719.
- Germann CA, Perron AD. Risk management and avoiding legal pitfalls in the emergency treatment of high-risk orthopedic injuries. Emerg Med Clin North Am 2010;28:969.
- Hodgkinson DW, Kurdy N, Nicholson DA, Driscoll PA. ABC of emergency radiology. The wrist. BMJ 1994;308:464-468.
- Davenport M, Tang P. Injuries to the hand and digits. In: Tintinalli JE, Stapczynski J, Ma O, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016.
- National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Available at: https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf. Accessed Jan. 16, 2017.
- Söderqvist A, Ekström W, Ponzer S, et al. Prediction of mortality in elderly patients with hip fractures: A two-year prospective study of 1,944 patients. Gerontology 2009;55:496-504.
- Haentjens P, Magaziner J, Colon-Emeric CS, et al. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann Intern Med 2010;152:380.
- Steele M, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, Stapczynski J, Ma O, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016.
- Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma 2003;17:53-56.
- Ritcey B, Pageau P, Woo MY, Perry JJ. Regional nerve blocks for hip and femoral neck fractures in the emergency department: A systematic review. CJEM 2016;18:37-47.
- Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: A randomized controlled trial. Acad Emerg Med 2013;20:584-591.
- Stephenson JW, Davis KW. Imaging of traumatic injuries to the hip. Semin Musculoskelet Radiol 2013;17:306-315.
- Wendt K, Heim D, Josten C, et al. Recommendations on hip fractures. Eur J Trauma Emerg Surg 2016;42:425-431.
- Auron-Gomez M, Michota F. Medical management of hip fracture. Clin Geriatr Med 2008;24:701-719, ix.
- Roberts KC, Brox WT, Jevsevar DS, Sevarino KL. Management of hip fractures in the elderly. J Am Acad Orthop Surg 2015;23:131-137.
- Shivji FS, Green VL, Forward DP. Anatomy, classification and treatment of intracapsular hip fractures. Br J Hosp Med (Lond) 2015;76:290-295.
- Shah S, Thomas AC, Noone JM, et al. Incidence and cost of ankle sprains in United States emergency departments. Sports Health 2016;8:547-552.
- Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa ankle rules. JAMA 1994;271:827.
- Stiell I, Wells G, Laupacis A, et al. Multicentre trial to introduce the Ottawa ankle rules for use of radiography in acute ankle njuries. BMJ 1995;311:594.
- David S, Gray K, Russell JA, Starkey C. Validation of the Ottawa ankle rules for acute foot and ankle injuries. J Sport Rehabil 2016;25:48-51.
- Jones P, Dalziel SR, Lamdin R, et al. Oral non-steroidal anti-inflammatory drugs versus other oral analgesic agents for acute soft tissue injury. Cochrane Database Syst Rev 2015;(7):CD007789.
- Kaminski TW, Hertel J, Amendola N, et al. National Athletic Trainers’ Association position statement: Conservative management and prevention of ankle sprains in athletes. J Athl Train 2013;48:528.
- Jones MH, Amendola AS. Acute treatment of inversion ankle sprains: Immobilization versus functional treatment. Clin Orthop Relat Res 2007;455:169.
- Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br J Sports Med 2017;51:113-125.
- Lamb SE, Marsh JL, Hutton JL, et al. Mechanical supports for acute, severe ankle sprain: A pragmatic, multicentre, randomised controlled trial. Lancet 2009;373:575.
- Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: A systematic review. Clin Orthop Relat Res 2007;455:93-101.
- Atkin DM, Fithian DC, Marangi KS, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 2000;28:472-479.
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-1121.
- Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: A randomized clinical trial.
J Bone Joint Surg Am 2008;90:463. - Patellofemoral instability and malalignment. In: Essentials of Musculoskeletal Care, 2nd ed. Snider RK. American Academy of Orthopedic Surgeons: Rosemont; 2001:387.
- Kocher MS. Intra-articular injuries of the knee. In: Rockwood and Wilkins’ Fractures in Children, 7th edition. Beaty JH, Kasser JR, eds. Lippincott, Williams & Wilkins: Philadelphia;2010:900.
- Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am 2003;34:385-396.
Orthopedic injuries are a common reason for emergency department (ED) visits. Orthopedic injuries should be diagnosed promptly and accurately and treated to optimize the outcome.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
