The Influenza Virus: Winter Is Coming
December 1, 2018
Reprints
AUTHORS
Gregory Sugalski, MD, Associate Professor, Department of Emergency Medicine, Rutgers New Jersey Medical School, Newark
Michael Ullo, MD, Resident Physician, EM PGY-3, Department of Emergency Medicine, Rutgers New Jersey Medical School, Newark
PEER REVIEWER
Catherine Marco, MD, FACEP, Professor, Emergency Medicine and Surgery, Wright State University, Dayton, OH
EXECUTIVE SUMMARY
- Most influenza in humans is caused by influenza A or B.
- Patients at risk for more severe disease include children, the elderly, pregnant women, and those with chronic neuromuscular or respiratory disease. Obese patients also are at risk.
- Antiviral treatment should be considered for hospitalized patients, those with severe disease, and those at risk of more severe disease.
- No guidelines exist to suggest which patients should be hospitalized. Patients with hypoxia, lung infiltrates, mental status changes, and significant risk factors should be considered for admission.
- Pediatric patients with influenza may present with symptoms of nausea and vomiting instead of typical upper respiratory symptoms.
Background
Influenza is an acute respiratory illness responsible for significant seasonal epidemics each year. The disease is transmitted by the influenza virus, an enveloped RNA virus that is part of the Orthomyxoviridae family. Despite commonly being a self-limited illness, the virus causes significant morbidity and mortality each year.
Influenza A and B are responsible for most clinically significant influenza infections. Influenza A is primarily implicated in significant pandemics that greatly affect public health. This virus is typed according to the antigenic characteristics of envelope glycoproteins, specifically hemagglutinin and neuraminidase. Influenza A has three major subtypes of hemagglutinin, H1, H2, and H3, along with two subtypes of neuraminidase, N1 and N2. Influenza B is not classified by subtypes and has not been shown to cause pandemics.
Additional subtypes of influenza, C and D, are associated with human disease less commonly. Influenza C produces a self-limited respiratory illness that is more common in children. Influenza D is believed to have originated in cattle and largely is responsible for bovine respiratory disease.1
The burden of influenza on the U.S. population each year is significant, with as many as 35.6 million cases since 2010 resulting in up to 56,000 deaths. Of the 35.6 million cases, as many as 710,000 patients were hospitalized secondary to influenza. The widespread use of the influenza vaccine continues to be the most effective method of prevention. The Centers for Disease Control and Prevention (CDC) estimates that the vaccine has prevented 5.1 million influenza illnesses, 2.5 million influenza-related medical visits, and 71,000 hospitalizations.2
Global Impact
Throughout history, several major global outbreaks of influenza have been documented. These outbreaks are due to the ability of viral cells to change their antigenic structure rapidly. While the influenza virus traditionally is regarded as a human disease entity, it is important to recognize that animals, such as birds and pigs, serve as important reservoirs for viral strains. These unique properties of the virus are responsible for the significant outbreaks that have shaped the history of public health.
Although the influenza pandemic of 1918 is perhaps the most well-known of all outbreaks, influenza has affected history for centuries. The first documented influenza outbreak may have occurred as early as 1510. While it would have been impossible for early historians to know the exact nature of the disease, this illness bore similar traits to the modern influenza virus that is well described today. Historical accounts of rapid-onset fever with respiratory symptoms that occurred via trade routes or in major population centers suggest that influenza epidemics and pandemics have been present throughout the course of human history.3
H1N1 Pandemic, 1918
The H1N1 avian influenza virus had a major worldwide impact from 1918-1919. Historical estimates suggest that nearly 500 million people across the globe were infected, representing roughly one-third of the entire population. In the United States, the virus emerged during the spring of 1918 when military personnel first were reported to have flu-like symptoms. Transmission of the virus resulted in the deaths of 50 million people worldwide, with roughly 675,000 deaths in the United States.4,5 In 2005, researchers successfully recreated the virus in an effort to learn more about the emergence of pandemic viruses.6
H2N2 Pandemic, 1957-1958
In February 1957, the H2N2 strain of the influenza A virus resulted in the pandemic known as the “Asian Flu.” Located predominantly in East Asia, the virus spread to coastal U.S. cities during the summer of 1957. Approximately 1.1 million deaths were documented worldwide, with close to 116,000 fatalities in the United States.7,8
H3N2 Pandemic, 1968
The H3N2 strain of the influenza A virus was documented to reach the United States in September 1968. The estimated number of deaths was 1 million worldwide, with roughly 100,000 fatalities in the United States.9
H1N1 Pandemic, 2009
In April 2009, a novel strain of the influenza A virus, H1N1, resulted in a significant outbreak of respiratory illness. The strain emerged in Mexico and quickly spread across the United States, with more than 55 million hospitalizations worldwide. Attempts to curb the infection resulted in the production of a specially formulated vaccine. The clinical impact of this virus resembled previous strains of influenza; however, there was increased morbidity among younger adults with comorbidities. In the United States, more than 10,000 patients died as a result of complications from infection. The World Health Organization declared the pandemic over in April 2010.10,11
H3N2 Variant Influenza, 2011
First identified in 2011, the H3N2 strain of the influenza A virus has been responsible for more than 400 cases of influenza, with the majority identified after July 2012.12 This strain was found to be swine in origin, with the addition of the M gene from the H1N1 influenza A virus. Most affected individuals reported contact with swine prior to illness. Cases of this strain typically are milder and self-limited.
Avian H7N9 Influenza, 2013
The novel avian H7N9 strain was identified first in China in 2013, and has been responsible for annual epidemics during influenza season. As with the H3N2 influenza strain, there is limited evidence of direct person-to-person transmission. Most cases have been associated with the handling of poultry prior to illness. Patients with confirmed avian H7N9 influenza had severe disease, with mortality rates from 27-36%, and pneumonia was a common complication.13,14
Epidemiology
The influenza virus carries a clinically significant health burden that tends to occur seasonally, with peak activity in the winter months. This phenomenon is associated with the antigenic shifts and antigenic drifts seen in the type A strain of the virus. Major changes in the virus’s glycoproteins (neuraminidase and hemagglutinin) are termed antigenic shifts. These shifts are responsible for the significant epidemics and pandemics that affect large populations. Minor changes in the structure of these glycoproteins result in antigenic drift, which tends to result in more localized outbreaks.
The incidence of influenza is difficult to characterize because the infection is not always diagnosed and the incidence varies based on the disease burden during each season or unique epidemic. Furthermore, the incidence varies based on differing age groups. The World Health Organization currently estimates that annual influenza epidemics result in 1 billion infections worldwide, with 3 to 5 million cases of severe disease.15 A meta-analysis of hospitalized patients in the United States suggests an annual incidence around 8%.16 Seasonal disease causes 250,000 and 500,000 deaths worldwide and between 5,000 to 50,000 deaths in the United States.17
Influenza Season
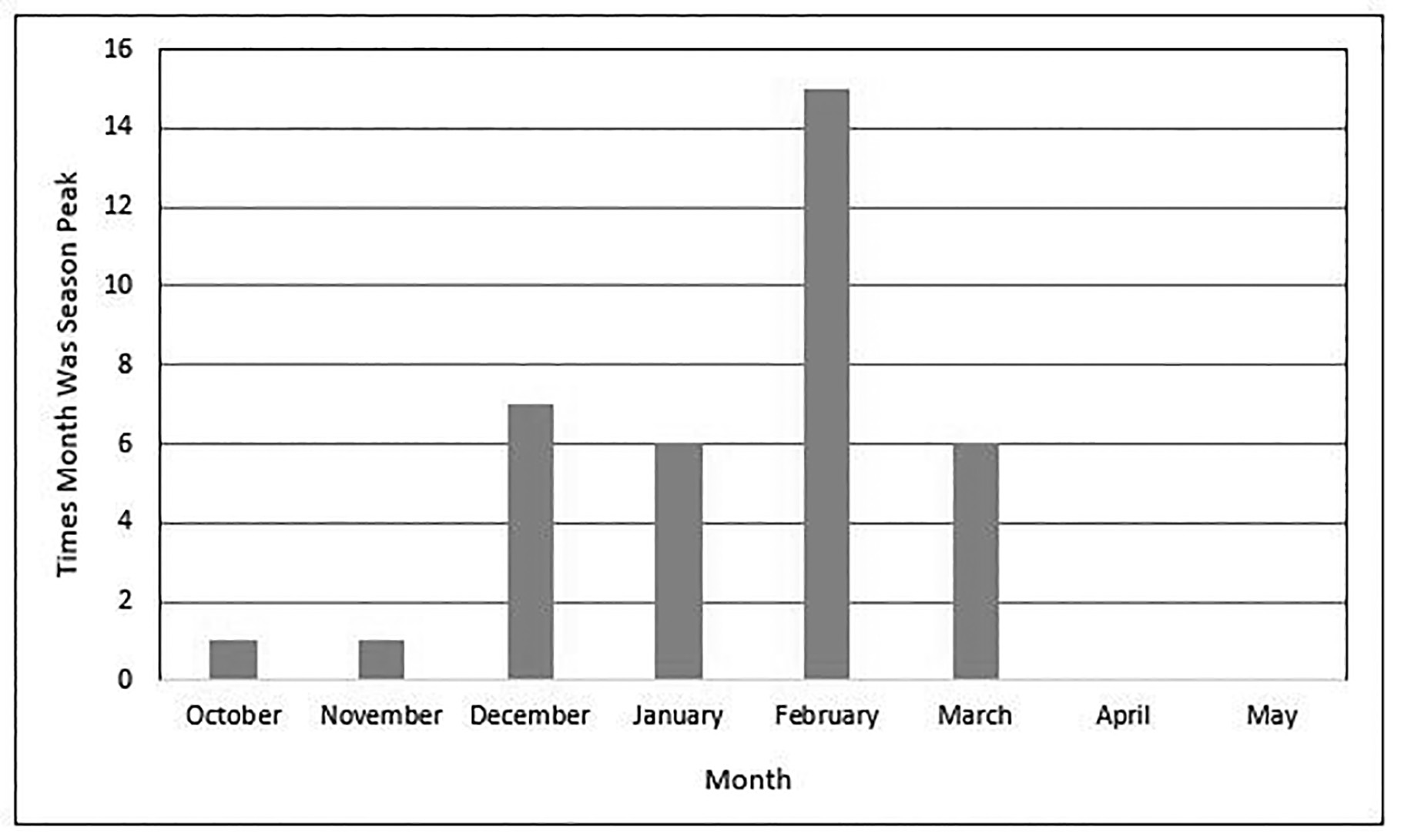
Although the influenza virus circulates year-round, “influenza season” typically is defined as the period when infection with the influenza virus is the highest. In the United States, the CDC maintains annual data with weekly influenza reports available to the public. The incidence of respiratory secretions testing positive for influenza begins to rise in October and peaks throughout the winter months in the Northern Hemisphere.18 (See Figure 1.) Despite this, it is important for the clinician to remember that influenza circulates continuously throughout the year and may be present at any time.
Figure 1. Peak Month of Influenza Activity 1982-1983 Through 2017-2018 |
 |
|
Source: Centers for Disease Control and Prevention |
Although the influenza season typically occurs during the winter months in both the Northern and Southern Hemispheres, influenza season may occur at any period during the year in tropical regions and may affect travelers. Similarly, sporadic outbreaks may occur on cruise ships and as a result of airline travel.19,20
Etiology
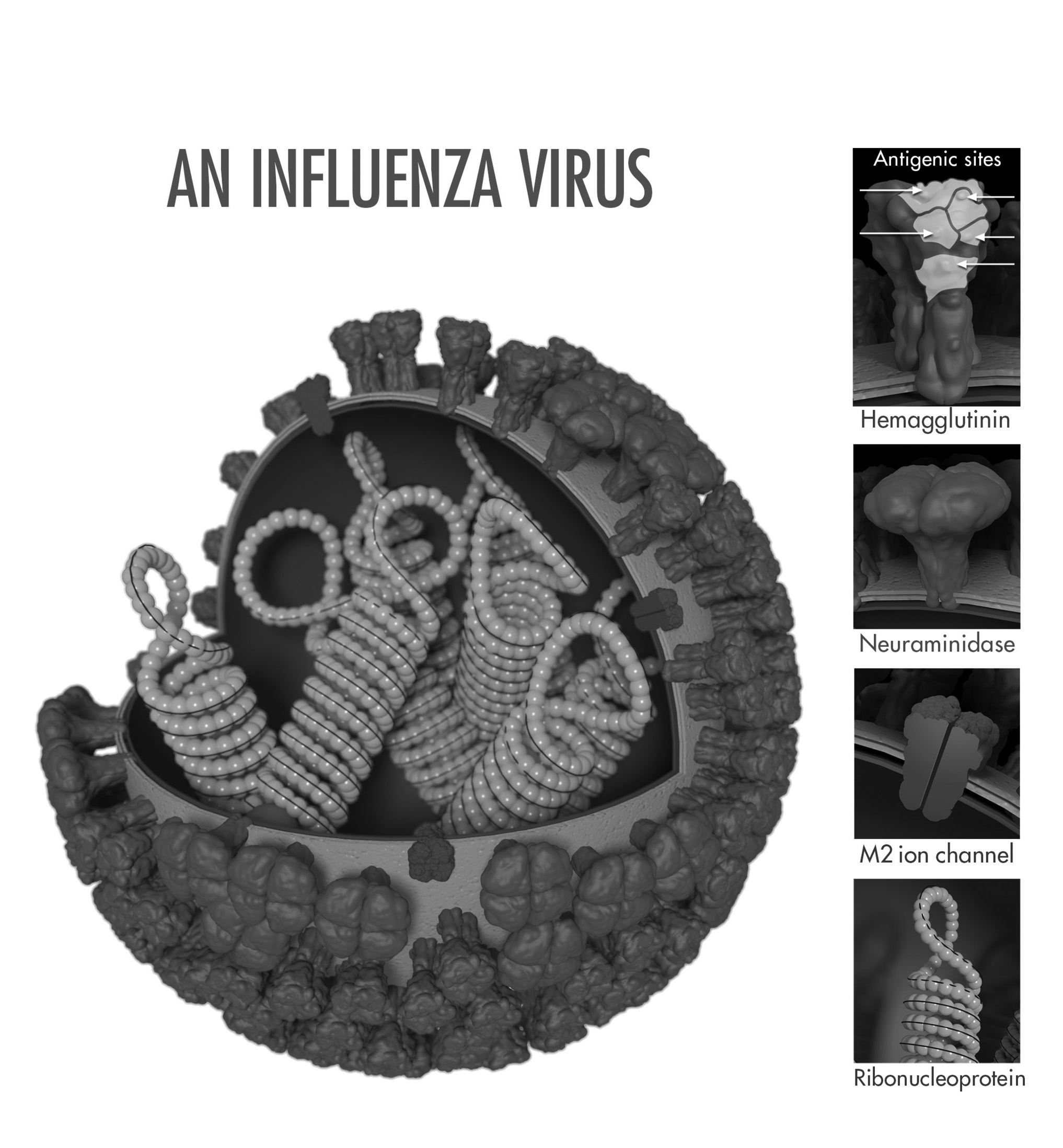
The influenza virus (genus influenzavirus) is a negative-sense, single-strand RNA virus. Influenza A, B, C, and D have been identified, with types A and B responsible for the bulk of human pathology. The A and B viral genome contains segments of genetic material that encodes viral proteins that facilitate viral replication and entry into host cells. The hemagglutinin protein allows for viral entry, while the neuraminidase protein allows for viral release. (See Figure 2.)
Figure 2. Influenza Virus |
 |
|
Source: CDC/Douglas Jordan; Dr. Ruben Donis, Dr. James Stevens, Dr. Jerry Tokars, Influenza Division; photo credit: Dan Higgins |
Risk Factors for Infection
Risk factors for infection are similar to the risk factors for other viral pathologies that cause disease in humans. Children without significant previous exposure to the virus are at a higher risk for infection with more severe features. Because of their decreased immune system function and significant medical comorbidities, the elderly are at higher risk for severe illness that often requires hospitalization.21
Patients with neuromuscular disease and lung pathology also are more susceptible to infection. This risk is thought to be due to impaired handling of respiratory secretions.22 Females who are pregnant have an increased risk throughout pregnancy, with a peak during the third trimester that persists through the postpartum period.23
Obese individuals are at higher risk of infection because of several proposed mechanisms. Reduced efficacy of vaccination as well as increased viral replication have been described in patients with a significantly elevated body mass index.24
Pathophysiology
Influenza virus is spread from person to person largely via large droplet transmission that occurs during sneezing and coughing. Transmission from host to recipient occurs when both parties are within close contact, typically less than six feet, as the large droplets do not remain aerosolized for significant periods of time.25 The virus also can spread by touching a surface contaminated with droplets and then touching mucous membranes, such as the conjunctiva of the eyes. Covering coughs and sneezes and good hand washing practices are critical to preventing transmission. The virus enters the respiratory tract and targets the epithelial cells for subsequent replication. The virus binds to the cell wall through an interaction between the virus’s hemagglutinin glycoprotein and sialic acid glycoproteins on the host cell wall. Once the virus enters the cell and replicates, the neuraminidase glycoprotein aids in the release of replicated virions. This process leads to eventual apoptosis of the affected cells and subsequent spread of the virus.
Infectious Course
The incubation period for influenza typically is one to four days. Viral shedding is thought to occur within 24 to 48 hours before symptom onset, although there is less of a viral burden than when the patient is symptomatic.25 Peak viral shedding has been shown to occur two days after transmission.26 Longer periods of shedding may occur with certain patient populations, such as children, older adults, immunocompromised patients, or those with chronic medical conditions.27-29
Uncomplicated influenza infection typically manifests with an acute onset of fever, headache, myalgias, and malaise. Following these initial symptoms, patients commonly experience symptoms associated with respiratory tract disease, such as cough, sore throat, and rhinorrhea.30 Patients with uncomplicated influenza usually recover from their illness within two to five days, although complete symptom resolution may take one week or more.
Clinical Presentation
The clinical presentation of uncomplicated influenza mimics other respiratory viral syndromes. Patients often present with the abrupt onset of symptoms within one to four days of exposure to the virus. Symptomatology can range from mild to life-threatening and can last for two weeks.31,32
Initial symptoms after infection include high fevers, intense myalgias, headaches, and anorexia. As infection progresses, patients tend to exhibit respiratory tract symptoms, such as nasal congestion, rhinorrhea, sore throat, and development of a nonproductive cough. The presence of gastrointestinal symptoms, such as vomiting and diarrhea, rarely is associated with influenza in adult patients. In contrast, nausea and vomiting may be key elements of the history elicited for pediatric patients.
The physical examination often is remarkable for fever with the presence of posterior cervical adenopathy and erythematous mucous membranes of the nasopharyngeal passages. The oropharynx may appear hyperemic, and the lung examination can vary from benign to rales secondary to superimposed pneumonia. Tachycardia may be present as a response to the febrile state or dehydration secondary to decreased oral intake. Children may demonstrate erythematous tympanic membranes suggestive of acute otitis media.
Patients at the extremes of age may present atypically. Exacerbations of underlying chronic medical comorbidities may be the initial presentation for older patients. Careful consideration should be applied when evaluating this subset of patients, as diagnosis is not always straightforward.11,31,32
Differential Diagnosis
Influenza carries a presentation similar to other viral syndromes and can be misdiagnosed.
A thorough history and physical examination by the emergency physician (EP) can help guide the evaluation of patients for potential etiologies. Upper respiratory infections caused by other viral agents, such as adenovirus, rhinovirus, and coronavirus, present similarly to influenza. (See Table 1.) Overlapping symptoms such as rhinorrhea, myalgias, and cough can predominate the clinical picture. Other infectious pathologies, such as meningitis, pneumonia, and pyelonephritis, should be considered in the evaluation of patients with influenza-like symptoms. A thorough travel history and exposure history should be pursued to screen for other etiologies such as dengue fever or Ebola. This broad differential can make diagnosis challenging for the EP.
Table 1. Cold vs. Flu |
||
|
Signs and Symptoms |
Common Cold |
Influenza |
|
Onset of symptoms |
Gradual |
Abrupt |
|
Fever |
Rare |
Usual |
|
Myalgias |
Slight |
Usual |
|
Chills |
Uncommon |
Fairly common |
|
Malaise |
Sometimes |
Usual |
|
Sneezing |
Common |
Sometimes |
|
Nasal congestion |
Common |
Sometimes |
|
Sore throat |
Common |
Sometimes |
|
Headache |
Rare |
Common |
|
Source: Adapted from: Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). Cold versus Flu. |
||
Diagnosis and Testing
Influenza can be diagnosed clinically based on a thorough history and physical examination without the need for routine diagnostic testing. The abrupt onset of a febrile respiratory illness with systemic symptoms such as myalgias and headaches during peak months can guide clinicians toward a presumptive diagnosis.33,34
Laboratory testing is available and should be reserved for instances in which confirmatory testing will affect patient care. According to the CDC, testing during an acute outbreak of respiratory illness can help determine if influenza is the cause and guide implementation of prevention and control measures.33
In infants and young children, nasal aspirates and swabs are the preferred specimens for testing. Specimens should be obtained from the nasopharynx in older children and adults. In mechanically ventilated patients, endotracheal aspirates or bronchiolar lavage fluid should be obtained for evaluation of the lower respiratory tract.35,36
Suggested uses for diagnostic testing include hospitalized patients, patients with significant medical comorbidities, and documentation for institutional purposes. Individual providers should contact their laboratory for detailed information regarding the performance of the specific diagnostic test used at their institution.
Rapid Antigen Testing
The rapid antigen test can identify viral nucleoprotein antigens in respiratory specimens.35 Data suggest that this testing method carries a pooled sensitivity of 62% and specificity of 98%.36 Although these tests can produce results in as quick as 15 minutes, they tend to have lower sensitivity than reverse transcriptase polymerase chain reaction (PCR). Rapid antigen testing in the emergency department (ED) has limited utility, as uncomplicated cases do not require diagnostic testing for presumptive treatment. Hospitalized patients should have PCR analysis performed.
Polymerase Chain Reaction
The PCR method of diagnosis typically is more burdensome because it can take approximately eight hours and is not always readily available. Despite this, PCR analysis may be useful in select patients, as sensitivity and specificity approach 100%.37
Viral Culture
Viral culture, typically viewed as the gold standard for diagnosis, has a turnaround time of 48-72 hours. Therefore, it is not used for initial clinical management in the emergency setting and instead may be more beneficial for public health screening.35
Complications
Patients with influenza also may develop more severe complications as a direct result of their infection. Well-established complications include primary influenza pneumonia, secondary bacterial pneumonia, myositis, rhabdomyolysis, acute myocardial infarction, myocarditis, pericarditis, central nervous system involvement, and toxic shock syndrome.
Although primary influenza pneumonia is one of the rarest complications of influenza infection, it is also one of the most severe. Clinicians should consider primary pneumonia in patients with persistent symptoms and recurrent fevers. Subsequent secondary bacterial pneumonia frequently is recognized as a complication in patients older than 65 years of age.38 Radiologic imaging of the chest can assist with diagnosis. Streptococcus pneumoniae is the most common bacteria implicated. Clinicians also should recognize the increasing prevalence of community-acquired methicillin-resistance Staphylococcus aureus as a causative agent.39,40
Management
The mainstay of management for most adults and children infected with the influenza virus remains supportive care, as the disease usually is self-limited. Otherwise healthy patients without significant comorbidities may achieve symptomatic relief with over-the-counter medications and adequate oral hydration.
Antiviral therapy, when initiated promptly, has been shown to play a role in shortening the duration of influenza symptoms. The greatest benefit of these medications has been demonstrated when given to febrile patients within the first 24 to 30 hours of presentation.41,42,43
The two major classes of antiviral medications for influenza are the neuraminidase inhibitors (oral oseltamivir, intranasal zanamivir, and intravenous peramivir) and adamantanes (oral amantadine and rimantadine). Because of concerns that adamantanes are effective only against influenza A, and most viral strains are highly resistant to this drug class, their routine use is not recommended. (See Table 2.) Consequently, neuraminidase inhibitors predominate as the antiviral therapy of choice when treating suspected or confirmed cases of influenza in the overwhelming majority of patients.44
Current clinical guidelines from the CDC and the Infectious Diseases Society of America (IDSA) recommend initiation of neuraminidase inhibitors as soon as possible with confirmed or suspected cases of influenza in patients with severe illness, hospitalized patients, and patients at high risk of complications. The decision to administer therapy should not be delayed or depend on results of diagnostic testing.44,45
Table 2. Neuraminidase Inhibitors in the Treatment of Influenza |
|||
|
Drug |
Indications |
Contraindications |
Common Adverse Effects |
|
Oseltamivir (Tamiflu) |
Seasonal influenza treatment in patients Seasonal influenza prophylaxis in patients ≥ 1 year of age |
Hypersensitivity to medication or component of formulation |
Headache, vomiting |
|
Zanamivir (Relenza) |
Seasonal influenza treatment in patients Seasonal influenza prophylaxis in patients ≥ 5 years of age |
Hypersensitivity to medication or component of formulation Avoid in patients with underlying respiratory disease (chronic obstructive pulmonary disease, asthma) |
Headache, sore throat, cough, rhinorrhea |
|
Peramivir (Rapivab) |
Seasonal influenza in patients 2 years of age and older |
Hypersensitivity to medication or component of formulation |
Hypertension, insomnia, increased serum glucose, constipation, diarrhea, increased alanine aminotransferase and aspartate aminotransferase |
|
Sources: Oseltamivir. Lexi-Drugs. Lexicomp. Wolter Kluwer Health, Inc. Riverwoods, IL. Available at: http://online.lexi.com; Zanamivir. Lexi-Drugs. Lexicomp. Wolter Kluwer Health, Inc. Riverwoods, IL. Available at: http://online.lexi.com; Peramivir: Lexi-Drugs. Lexicomp. Wolter Kluwer Health, Inc. Riverwoods, IL. Available at: http://online.lexi.com. |
|||
Otherwise healthy adults and children with presumed or confirmed influenza may be treated electively as outpatients with neuraminidase inhibitors. Studies in these populations demonstrated a small decrease in length of illness by approximately one day in adults.46 Shared decision-making with the patient on a case-by-case basis can help guide the decision to initiate medical therapy.
Oseltamivir (Tamiflu) is one of the most frequently prescribed medications used in the management of influenza. The typical dosage regimen for oseltamivir is described in Table 3. Adult patients with a creatinine clearance less than 60 should have their dose adjusted to 30 mg twice daily.47 In addition, patients with creatinine clearance ≤ 30 should have their dose reduced to 30 mg one time daily. Although the drug is considered pregnancy class C, the American College of Obstetricians and Gynecologists (ACOG) recommends presumptive treatment with antiviral medication during pregnancy.44 Treatment should be initiated within 48 hours of onset of illness and continued for a duration of five days. Common side effects include headache, nausea, and vomiting.
Table 3. Oseltamivir Dosing for Treatment, Not for Prophylaxis |
|
|
Adults |
• 75 mg twice daily for 5 days |
|
Children (> 1 year of age) |
• < 15 kg: 30 mg twice daily for 5 days • 15 to 23 kg: 45 mg twice daily for 5 days • 23 to 40 kg: 60 mg twice daily for 5 days • > 40 kg: 75 mg twice daily for 5 days |
|
Infants (< 1 year of age) |
• 1 to 8 months: 3 mg/kg/dose twice daily • 9 to 11 months: 3.5 mg/kg/dose twice daily |
|
Source: Oseltamivir. Lexi-Drugs. Lexicomp. Wolters Kluwer Health, Inc. Riverwoods, IL. Available at: http://online.lexi.com. |
|
Patients who require hospitalization or who are deemed to be at high risk for influenza complications should be treated with a neuraminidase inhibitor regardless of duration of symptoms. These risk factors include age older than 65 years, pregnancy, and chronic comorbid medical conditions. Initiation of therapy should not be delayed while awaiting diagnostic or confirmatory testing.44,48
Resuscitation of the critically ill patient initially should focus on the ABCs of emergency medicine management: airway, breathing, and circulation. A stepwise approach should be taken toward resuscitation, with prompt attention to abnormal vital signs and simultaneous expediting of therapeutic modalities. Endotracheal intubation may be necessary if patients present with profound hypoxia and/or respiratory distress that is not responsive to noninvasive management such as supplemental oxygen. The potentially septic patient should be monitored carefully and treated with crystalloid resuscitation if hypotension and/or tachycardia are present. Initiation of vasopressors may be considered in patients who remain hypotensive despite adequate resuscitation with intravenous fluids for hemodynamic support.
Chemoprophylaxis for patients with exposure to suspected or confirmed cases of influenza remains controversial. In general, routine use of chemoprophylaxis with antivirals is not recommended. Patients exposed to influenza who are at high risk for complications and cannot be vaccinated because of contraindications should be considered as candidates.44
Emerging Therapy
In October 2018, the United States Food and Drug Administration (FDA) announced approval of single-dose baloxavir marboxil (Xofluza) for treatment of acute, uncomplicated influenza in people 12 years of age and older.49 This oral medication works by blocking mRNA synthesis of endonucleases responsible for viral proliferation.50 Results from a randomized, controlled trial comparing baloxavir marboxil to oseltamivir and placebo demonstrated superiority in reduction of viral load one day after initiation of pharmacotherapy for patients receiving baloxavir marboxil.51 It remains unclear whether baloxavir marboxil is superior to oseltamivir for hospitalized or immunocompromised patients, or in those with neuraminidase inhibitor-resistant influenza infections.52
Prevention
Vaccination remains the cornerstone for primary prevention of influenza. Although the vaccine is effective in preventing infection with common strains of the virus, there remains significant potential for illness despite vaccination.53
Given the high rates of new strains that develop from significant antigenic variation, vaccines are reformulated annually to match expected circulating strains. These formulations generally are developed six months prior to influenza season based on surveillance data from the previous year.
The seasonal influenza vaccine is recommended for yearly administration in patients 6 months of age and older who do not have any known contraindications for vaccination. This includes pregnant women (regardless of gestational age) and women who are breastfeeding.54
Currently, three types of influenza vaccines are available in the United States:
- The inactivated influenza vaccine is administered intramuscularly and is available in tetravalent and quadrivalent forms for patients 6 months of age and older.
- The recombinant hemagglutinin vaccine is available for patients 18 years of age and older.
- The intranasal, live attenuated influenza vaccine is available for otherwise healthy and nonpregnant patients, 2-49 years of age.
These preparations typically are available in the fall to prepare for peak incidence during the winter months.55,56 In addition, a high-dose vaccine is available for patients older than 65 years of age.
Contraindications to vaccination include severe allergy to previous formulations of the influenza vaccine in the past. Additionally, several of the available forms of the vaccine contain small amounts of egg protein. Previously, egg allergy was considered to be a contraindication to vaccination; however, recent data have demonstrated that vaccination may be given in patients with known egg allergy with appropriate precautions. These patients should be referred to an allergy specialist for additional evaluation prior to administration.
The intranasal, live attenuated vaccine should be withheld from patients who are immunocompromised. This vaccine also is contraindicated in patients who are pregnant, 50 years of age or older, and those who have taken influenza antiviral medication within the past 48 hours.56
Recently, research efforts have focused on the establishment of a universal vaccination. This vaccine would function to elicit the creation of protective antibodies in vaccinated patients against well-conserved viral proteins.57,58
Disposition
Outpatient Management
Most patients diagnosed with influenza from the ED may be discharged home safely with strong return precautions. Patients discharged from the ED should follow up with a primary care provider in two days for re-evaluation for monitoring of their clinical course. Vital signs should be re-evaluated prior to discharge planning to check for persistent hypoxia, tachycardia, or tachypnea. The febrile state is expected with the disease process, and clinicians should consider the effects of administration of antipyretics when evaluating the significance of fever in the ED.
Discharge instructions should educate patients on signs and symptoms that should prompt a patient to seek immediate medical attention. Patients should be instructed to return to the ED if they experience persistent fever, inability to tolerate oral intake, confusion, or changes in mental status. Upon discharge, patients diagnosed with influenza should be educated on hand washing, respiratory hygiene, and cough etiquette to decrease the risk of viral spread.
Supportive care with antipyretics, rest, and hydration are the mainstays of outpatient therapy. Treatment with an antiviral agent may be initiated without diagnostic testing in the appropriate clinical setting. Patients should be counseled regarding the risks and benefits of medical therapy before initiation with a neuraminidase inhibitor.
Observation
Certain patients may benefit from observation in the hospital or ED depending on institutional practices. Patients should be placed on droplet precautions to limit the spread of viral illness within the healthcare facility.59 The observation setting may be a useful disposition for patients who may benefit from serial cardiopulmonary examinations and/or intravenous hydration secondary to clinically significant dehydration. Patients at the extremes of age without significant medical comorbidities may benefit from this extended period of medical observation. Prior to discharge, patients should be re-evaluated for symptomatic improvement and the ability to tolerate oral intake. If a patient’s clinical response to symptomatic therapy fails to improve, strong consideration should be given for admission to the hospital for further management.
Hospitalization
During the past eight years, more than 700,000 patients have required hospitalization secondary to known or suspected influenza infection.2 The decision to admit a patient to the hospital for influenza can be particularly challenging, as no well-validated scoring system exists to guide disposition. This decision should be based on clinical judgment in conjunction with assessment of the patient’s risk factors.
A subset of patients presenting to the ED should be considered for admission to the hospital because of concern for decompensation from the viral illness. Adults older than 65 years of age, pregnant women, children younger than 5 years of age, as well as individuals with comorbid conditions48 should be considered for admission. (See Table 4.) Additionally, patients previously evaluated by a medical provider who have failed to improve with outpatient management should be considered for admission.
Table 4. Comorbid Conditions That Increase Risk of Influenza Complications |
|
|
Source: Fiore AE, Fry A, Shay D, et al. Antiviral agents for the treatment and chemoprophylaxis of influenza — recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60:1-24 |
Patients with influenza may deteriorate and develop acute respiratory distress syndrome (ARDS), requiring possible intubation and intensive care for hypoxemic respiratory failure. In these patients, extracorporeal membrane oxygenation (ECMO) may serve as bridge therapy during the acute illness.60 The EP should proceed cautiously with patients who present with hypoxia because these patients may progress to respiratory failure. Patients who are deemed to be at high risk because of comorbidities or changes in mental status should be screened for intensive care admission when available. Consultation with a pulmonologist or infectious disease specialist may be appropriate depending on the patient’s clinical course or past medical history.
Summary
Influenza outbreaks occur each year, with their nature and extent largely determined by the virus’s glycoprotein structure and antigenic properties. These outbreaks typically occur during the winter months and can confer high morbidity to the general patient population. Increased mortality rates are seen in young children, older adults, and those with chronic comorbid medical conditions.
During the winter months, EPs should maintain a high suspicion for influenza in all patients presenting with an acute febrile respiratory illness. Although the differential diagnosis is broad, the history and physical examination can guide the EP toward a presumptive diagnosis without the need for additional testing. Laboratory testing is available and should be reserved for those cases in which the diagnosis may change the clinical management.
Treatment is indicated for patients with severe disease or those at risk for complications. Initiation of antiviral treatment should be within 48 hours of symptom onset. Most otherwise healthy patients can be managed with supportive care only. Complicated cases of influenza may require hospitalization and treatment with antiviral therapy regardless of symptom duration.
Prevention of the influenza virus is achieved primarily through the annual influenza vaccine. This vaccine is formulated to protect patients from the most commonly circulating strains of the virus. This is accomplished by obtaining routine surveillance data about viral characteristics during each influenza season.
Emerging therapy, including single-dose antiviral medications and universal vaccination, may shape the rapidly evolving nature of the influenza virus and its burden on human health.
REFERENCES
- Flynn O, Gallagher C, Mooney J, et al. Influenza D virus in cattle, Ireland. Emerg Infect Dis 2018;24:389-391.
- Reed C, Chaves SS, Daily Kirley P, et al. Estimating influenza disease burden from population-based surveillance data in the United States. PloS One 2015;10:e0118369.
- Morens DM, Taubenberger JK, Folkers GK, Fauci AS. Pandemic influenza’s 500th anniversary. Clin Infect Dis 2010;51:1442-1444.
- Jester B, Uyeki T, Jernigan D. Readiness for responding to a severe pandemic 100 years after 1918. Am J Epidemiol 2018; doi: 10.1093/aje/kwy165. [Epub ahead of print].
- Belser JA, Tumpey TM. The 1918 flu, 100 years later. Science 2018;359:255.
- Centers for Disease Control and Prevention. Reconstruction of the 1918 influenza pandemic virus. Available at: https://www.cdc.gov/flu/about/qa/1918flupandemic.htm. Accessed Nov. 7, 2018.
- Viboud C, Simonsen L, Fuentes R, et al. Global mortality impact of the 1957-1959 influenza pandemic. J Infect Dis 2016;213:738-745.
- Langmuir AD. Epidemiology of Asian influenza. With special emphasis on the United States. Am Rev Respir Dis 1961;83:2-14.
- Glezen WP. Emerging infections: Pandemic influenza. Epidemiol Rev 1996;18:64-76.
- Reed C, Angulo FJ, Swerdlow DL, et al. Estimates of the prevalence of pandemic (H1N1) 2009, United States, April–July 2009. Emerg Infect Dis 2009;15:2004-2007.
- Walls RM, Hockberger RS, Gausche-Hill M. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Philadelphia: Elsevier; 2018.
- Outbreak of influenza A(H3N2) variant virus infections among persons attending agricultural fairs housing infected swine in Michigan and Ohio, July-August 2016. Pediatr Infect Dis J 2017;36:400.
- Gao R, Cao B, Hu Y, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 2013;368:1888-1897.
- Yu H, Cowling BJ, Feng L, et al. Human infection with avian influenza A H7N9 virus: An assessment of clinical severity. Lancet 2013;382:138-145.
- World Health Organization. Influenza (Seasonal) Fact Sheet. March 30, 2018. Available at: https://www.who.int/en/news-room/fact-sheets/detail/influenza-(seasonal). Accessed Nov. 8, 2018.
- Tokars JI, Olsen SJ, Reed C. Seasonal incidence of symptomatic influenza in the United States. Clin Infect Dis 2018;66:1511-1518.
- Takhar SS, Moran GJ. Serious viral infections. In: Tintinalli JE, Stapczynski JS, Ma OJ, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th edition. New York: McGraw-Hill; 2016: 1039.
- Centers for Disease Control and Prevention. Influenza: The flu season. Available at: www.cdc.gov/flu/about/season/flu-season.htm. Accessed Nov. 8, 2018.
- Moura FE. Influenza in the tropics. Curr Opin Infect Dis 2010;23:415-420.
- Brownstein JS, Wolfe CJ, Mandl KD. Empirical evidence for the effect of airline travel on inter-regional influenza spread in the United States. PLoS Med 2006;3:e401.
- Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA 2004;292:1333-1340.
- Keren R, Zaoutis TE, Bridges CB, et al. Neurological and neuromuscular disease as a risk factor for respiratory failure in children hospitalized with influenza infection. JAMA 2005;294:2188-2194.
- Neuzil KM, Reed GW, Mitchel EF, et al. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol 1998;148:1094-1102.
- Van Kerkhove MD, Vandemaele KA, Shinde V, et al. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: A global pooled analysis. PLoS Med 2011;8:e1001053.
- Brankston G, Gitterman L, Hirji Z, et al. Transmission of influenza A in human beings. Lancet Infect Dis 2007;7:257-265.
- Nonpharmaceutical interventions for pandemic influenza, international measures. Emerg Infect Dis 2006;12:81-87.
- Carrat F, Vergu E, Ferguson NM, et al. Timelines of infection and disease in human influenza: A review of volunteer challenge studies. Am J Epidemiol 2008;167:775-785.
- Leekha S, Zitterkopf NL, Espy MJ, et al. Duration of influenza A virus shedding in hospitalized patients and implications for infection control. Infect Control Hosp Epidemiol 2007;28:1071-1076.
- Klimov AI, Rocha E, Hayden FG, et al. Prolonged shedding of amantadine-resistant influenza A viruses by immunodeficient patients: Detection by polymerase chain reaction-restriction analysis. J Infect Dis 1995;172:1352-1355.
- Loeb M, Singh PK, Fox J, et al. Longitudinal study of influenza molecular viral shedding in Hutterite communities. J Infect Dis 2012;206:1078-1084.
- Cohen YZ, Dolin R. Influenza. In: Kasper DL, Fauci AS, Hauser SL, et al, (eds). Harrison’s Principles of Internal Medicine, 19th ed. New York: McGraw Hill Education; 2015:1209.
- Centers for Disease Control and Prevention. Clinical signs and symptoms of influenza. Available at: https://www.cdc.gov/flu/professionals/acip/clinical.htm. Accessed Nov. 8, 2018.
- Centers for Disease Control and Prevention. Information for clinicians on rapid diagnostic testing for influenza. Available at: http://www.cdc.gov/flu/professionals/diagnosis/rapidclin.htm. Accessed Nov. 8, 2018.
- Centers for Disease Control and Prevention. Influenza signs and symptoms and the role of laboratory diagnostics. Available at: http://www.cdc.gov/flu/professionals/diagnosis/labrolesprocedures.htm. Accessed Nov. 8, 2018.
- Chartrand C, Leeflang MM, Minion J, et al. Accuracy of rapid influenza diagnostic tests: A meta-analysis. Ann Intern Med 2012;156:500.
- Harper SA, Bradley JS, Englund JA, et al; Expert Panel of the Infectious Diseases Society of America. Seasonal influenza in adults and children — Diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: Clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2009;48:1003-1032.
- Abraham MK, Perkins J, Vilke GM, Coyne CJ. Influenza in the emergency department: Vaccination, diagnosis, and treatment: Clinical practice paper approved by American Academy of Emergency Medicine Clinical Guidelines Committee. J Emerg Med 2016;50:536-542.
- Chertow DS, Memoli MJ. Bacterial coinfection in influenza: A grand rounds review. JAMA 2013;309:275.
- Wolter N, Tempia S, Cohen C, et al. High nasopharyngeal pneumococcal density, increased by viral coinfection, is associated with invasive pneumococcal pneumonia. J Infect Dis 2014;210:1649-1657.
- Schwarzmann SW, Adler JL, Sullivan RJ Jr, Marine WM. Bacterial pneumonia during the Hong Kong influenza epidemic of 1968-1969. Arch Intern Med 1971;127:1037.
- Cooper NJ, Sutton AJ, Abrams KR, et al. Effectiveness of neuraminidase inhibitors in treatment and prevention of influenza A and B: Systematic review and meta-analyses of randomised controlled trials. BMJ 2003;326:1235.
- Heneghan CJ, Onakpoya I, Thompson M, et al. Zanamivir for influenza in adults and children: Systematic review of clinical study reports and summary of regulatory comments. BMJ 2014;348:g2547.
- Dobson J, Whitley RJ, Pocock S, Monto AS. Oseltamivir treatment for influenza in adults: A meta-analysis of randomised controlled trials. Lancet 2015;385:1729.
- Centers for Disease Control and Prevention. Influenza antiviral medications: Summary for clinicians. Available: http://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm. Accessed Nov. 8, 2018.
- Harper SA, Bradley JS, Englund JA, et al. Seasonal influenza in adults and children — Diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: Clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2009;48:1003-1032.
- Jefferson T, Demicheli V, Deeks J, Rivetti D. Neuraminidase inhibitors for preventing and treating influenza in healthy adults. Cochrane Database Syst Rev 2000;2:CD001265.
- Oseltamivir. Lexi-Drugs. Lexicomp. Wolters Kluwer Health, Inc. Riverwoods, IL.
- Fiore AE, Fry A, Shay D, et al. Antiviral agents for the treatment and chemoprophylaxis of influenza — recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60:1-24.
- Food and Drug Administration. FDA approves new drug to treat influenza [news release]. Oct. 24, 2018. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624226.htm. Accessed Nov. 8, 2018.
- Heo YA. Baloxavir: First global approval. Drugs 2018;78:693-697.
- Hayden FG, Sugaya N, Hirotsu N, et al. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med 2018;379:913-923.
- Uyeki TM. A step forward in the treatment of influenza. N Engl J Med 2018;379:975-977.
- Kilbourne ED. Influenza immunity: New insights from old studies. J Infect Dis 2006;193:7-8.
- [No authors listed]. ACOG Committee Opinion No. 732: Influenza vaccination during pregnancy. Obstet Gynecol 2018;131:e109-e114.
- Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2018–19 Influenza Season. MMWR Recomm Rep 2018;67:1-20.
- Committee on Infectious Diseases. Recommendations for prevention and control of influenza in children, 2017-2018. Pediatrics 2017;140: doi: 10.1542/peds.2017-2550.
- Lambert LC, Fauci AS. Influenza vaccines for the future. N Engl J Med 2010;363:2036-2044.
- Erbelding EJ, Post DJ, Stemmy EJ, et al. A universal influenza vaccine: The strategic plan for the National Institute of Allergy and Infectious Diseases. J Infect Dis 2018;218:347-354.
- Centers for Disease Control and Prevention. Prevention strategies for seasonal influenza in healthcare settings. Available at: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm. Accessed Nov. 8, 2018.
- Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators, Davies A, Jones D, Bailey M, et al. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA 2009;302:1888.
Influenza is an acute respiratory illness responsible for significant seasonal epidemics each year. Despite commonly being a self-limited illness, the virus causes significant morbidity and mortality. During the winter months, emergency physicians should maintain a high suspicion for influenza in patients presenting with an acute febrile respiratory illness.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
