By Michael Rubin, MD
Professor of Clinical Neurology, Weill Cornell Medical College
Brentuximab, an antibody-drug conjugate for the treatment of lymphomas, carries a high risk of inflammatory sensory and motor neuropathies.
Matthys A, Bardel B, Le Bras F, et al. Rate and characteristics of inflammatory neuropathies associated with brentuximab vedotin therapy. Eur J Neurol 2024; Mar 21. doi: 10.1111/ene.16285. [Online ahead of print].
Granted accelerated approval in 2011 by the U.S. Food and Drug Administration for the treatment of CD30-positive lymphomas such as Hodgkin’s and systemic anaplastic large cell lymphoma, brentuximab vedotin (BV) is a CD30-specific antibody-drug conjugate. To increase its potency, a cytotoxic drug (in this instance, the anti-tubulin agent monomethyl auristatin E [MMAE]) is linked to a monoclonal antibody, allowing the monoclonal antibody (which is specific for an antigen highly expressed on cancer cells) to specifically deliver the cytotoxic agent to the cancer, thereby sparing healthy tissue.
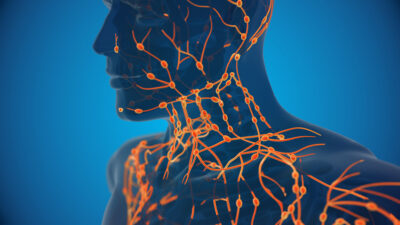
Infusion reactions are uncommon, anaphylaxis has been reported, and progressive multifocal leukoencephalopathy is rare. The most significant adverse event prompting treatment interruption is sensory neuropathy, occurring in 36% of participants in the Phase I trial and 42% of participants in the Phase II trial, with motor neuropathy occurring in 11% of participants. More than 70% of participants developed sensory neuropathy when BV was combined with either doxorubicin [Adriamycin], bleomycin, vinblastine, and dacarbazine (ABVD) or doxorubicin, bleomycin, and dacarbazine (AVD) for Hodgkin’s lymphoma. Rarely, cases of acute or chronic inflammatory neuropathy (BV-IN) have been reported, which may be reversed with immunotherapy and BV withdrawal. How quickly does BV-IN neuropathy develop and what are its risk factors and warning signs?
A retrospective review of all BV patients treated between April 2014 and September 2021 at the Lymphoid Malignancies Unit and Dermatology Department of Henri Mondor University Hospital, Créteil, France, was undertaken. BV neuropathy was defined as sensory or motor symptoms with onset or worsening while taking BV or up to three months following the last infusion. It was classified as inflammatory neuropathy if motor nerve conduction studies showed demyelinating neuropathy based on European Academy of Neurology/Peripheral Nerve Society (EAN/PNS) 2021 guidelines. Statistical analysis comprised Fisher’s exact test, the Wilcoxon rank-sum test, and chi-squared tests, with P < 0.05 deemed significant.
Among 85 BV-treated patients in the cohort, two patients were excluded because of the absence of reports. The median age was 55 years, the median number of BV infusions was six, and the median total dose was 696 mg. Four patients had preexisting neuropathy from prior chemotherapy and seven patients from unknown or mixed etiology (chemotherapy, alcohol, diabetes, or renal failure), two patients had carpal tunnel syndrome, and one patient had remote poliomyelitis.
BV-induced neuropathy was seen in 49% (n = 41) within a median of 10 weeks, of which six patients had BV-IN, representing 7.2% of BV-treated patients, or 14.6% of those with BV-induced neuropathy. Compared to those with classic BV-induced neuropathy, which was sensory predominant, progressive, and evolving into a classic stocking-glove distribution of paresthesia or pain, those with BV-IN had more frequent acute or subacute onset, were more frequently severe based on Common Terminology Criteria for Adverse Events grade, and had more frequent muscle weakness or abnormal gait presentation, either caused by ataxia or weakness, with diffuse areflexia, although reflex examination was poorly reported among the other patients to reach statistical significance. BV-IN may be more quickly recognized by identifying these four red flags in BV-treated patients presenting with neuropathy.
COMMENTARY
Brentuximab consists of three components: the human-CD30-specific chimeric immunoglobulin G1 monoclonal antibody (mAb) cAC10, the microtubule-disrupting agent MMAE, and a protease-cleavable covalent linker, which binds the two together. Brentuximab vedotin requires Chinese hamster ovary cells for production of the mAb, while the small-molecule components are chemically synthesized. In vivo, cAC10 binds to CD30 at the cancer cell surface, undergoing endocytosis and fusion with lysosomes where the linker is cleaved by lysosomal cysteine proteases, allowing MMAE to be released into the cancer cell, resulting in cancer cytotoxicity while sparing healthy tissue.1
REFERENCE
- Al Sbihi A, Alasfour M, Pongas G. Innovations in antibody-drug conjugate (ADC) in the treatment of lymphoma. Cancers (Basel) 2024;16:827.