CDC Publishes Guide to Help Hospitals Diagnose, Treat Sepsis
By Jonathan Springston, Editor, Relias Media
The Centers for Disease Control and Prevention (CDC) has published new guidance to help U.S hospitals implement, monitor, and optimize sepsis programs.
The Hospital Sepsis Program Core Elements includes seven pillars upon which to build a strong program: leadership commitment, accountability, multiprofessional expertise, action, tracking, reporting, and education. CDC officials hope medical facilities can use these resources to prevent sepsis, appropriately and quickly treat these cases, lower associated mortality rates and healthcare costs, and shorten lengths of stay.
The recently published results of a CDC-led national survey of more than 5,200 U.S. hospitals revealed some facilities have built their own sepsis programs. As of 2022, the CDC reported, 73% of respondents had created a sepsis program, ranging from 53% among hospitals with 0-25 beds to 95% among hospitals with more than 500 beds. A little more than half (55%) of respondents provide sepsis program leaders with dedicated time to manage the program and conduct daily activities.
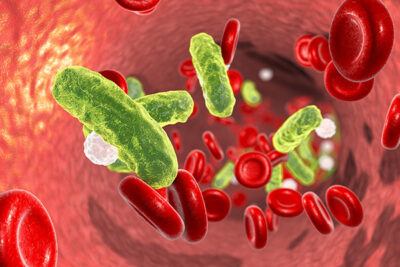
Despite some promising indicators, the CDC reported sepsis is responsible for at least 1.7 million adult hospitalizations and at least 350,000 deaths annually.
“Sepsis is taking too many lives. One in three people who dies in a hospital has sepsis during that hospitalization. Rapid diagnosis and immediate appropriate treatment, including antibiotics, are essential to saving lives, yet the challenges of awareness about and recognition of sepsis are enormous. That’s why CDC is calling on all U.S. hospitals to have a sepsis program and raise the bar on sepsis care by incorporating these seven core elements,” said CDC Director Mandy Cohen, MD, MPH.
In the August 2023 issue of ED Management, authors Dorothy Brooks and Stacey Kusterbeck produced a package of articles about how some emergency medicine practitioners are improving sepsis care through advanced diagnostic tools and a provider in triage model. For more on this and related subjects, be sure to read the latest issues of Critical Care Alert, Emergency Medicine Reports, Healthcare Risk Management, Hospital Infection Control & Prevention, and Infectious Disease Alert.
