
Falls in Older Adults
July 1, 2024
Reprints
AUTHORS
Mara O’Sullivan, MD, Department of Emergency Medicine, Wright State University Boonshoft School of Medicine, Kettering, OH
Andrea L. Kaelin, MD, MPH, FAAEM, FAEMUS, RDMS, CEPH, Assistant Professor, Emergency Medicine, Wright State University Boonshoft School of Medicine, Kettering, OH
Ashley A. Brent, MD, Department of Pathology, University of Michigan, Ann Arbor, MI
PEER REVIEWER
Steven M. Winograd, MD, FACEP, Attending Emergency Physician, Trinity, Samaritan Hospital, Troy, New York, NY
EXECUTIVE SUMMARY
- Falls in the older adult population require an assessment of the potential trauma and the cause of the fall. Common causes include syncope, polypharmacy, and infection.
- Cervical spine fracture is more common in older adult patients. Fractures are most common at C1-C4 and may have little pain associated. Computed tomography is the gold standard for imaging.
- Many older adults take anticoagulation medications. Reversal agents exist for warfarin (4-factor prothrombin complex concentrate) and several of the direct oral anticoagulants. However, the risk of further bleeding should be weighed with the risk of reversing the anticoagulation and exposing the patient to the underlying disease.
- Discharge from the emergency department requires assessment of the home situation, consultation with the family, and prevention of future falls.
Each year, there are about 3 million emergency department (ED) visits and 1 million hospitalizations related to falls in older adults.1 Fatal and nonfatal falls in patients older than 65 years of age cost an estimated $49.5 billion in 2015, a 32% increase in healthcare dollar expenditures compared to the previous year.2
Falls cause significant morbidity and mortality among older adult patients compared to younger patients.3-5 When treating a patient who has fallen, the emergency medicine physician should identify traumatic injuries and evaluate for medical pathology contributing to the fall, as well as manage the patient.
Older adults are a vulnerable population with communication barriers that may include regional language barriers, speech or hearing deficits, history by proxy from a living facility or caregivers, and dementia. Numerous comorbidities convey a higher risk for serious pathology associated with age. Emergency medicine clinicians need to have a high index of suspicion for serious pathology, even after a low-mechanism trauma.
Definition of the Problem
This article focuses on ground level falls in adults older than 65 years of age who present to the ED. The older adult population is the fastest growing subset in the United States, and 10% to 15% of ED presentations are falls in geriatric patients.6 More than one in four older adults fall annually, and there is an increasing mortality rate and admission rate in U.S. older adults who fall.1,6
Traumatic injuries are the result of the mechanical component of a fall, such as intracerebral hemorrhage and long bone fractures. Medical issues (i.e., seizure, stroke, or hypoglycemia) may be contributive, causing fall conditions. Medical conditions also complicate subsequent medical management, such as anticoagulation therapies, medical devices that are not compatible with magnetic resonance imaging (MRI), or underlying chronic obstructive pulmonary disease (COPD) in the management of rib fractures. Each workup and evaluation should be tailored to the patient’s specific presentation and comorbidities. A thorough history should include emergency medical services (EMS), family, or facility history of the patient at baseline and the situation surrounding the incident. All patients should receive a comprehensive physical examination to avoid delayed medical or traumatic diagnoses.
Etiology and Epidemiology
Older adult patients have greater injury severity scores than younger patients with comparable mechanisms of injury. Higher injury severity scores are largely due to association with the comorbid medical conditions of COPD, ischemic heart disease, diabetes, cirrhosis, and coagulopathies.7 Almost 95% of all hip fractures are caused by falls.8
Mortality from falls, especially in those older than 75 years of age, continues to trend upward.7,9 In 2016, 116.4 per 100,000 men and 105.9 per 100,000 women died with falls as the underlying cause of death.9 Predictors of mortality, independent of age, for older adults with an injury severity score (ISS) of > 16 include Glasgow Coma Scale (GCS) score ≤ 8, international normalized ratio (INR) > 1.4, a base excess ≥ -6, and acidosis.10 Older adult patients experience additional complications that lead to age-related higher mortality during post-trauma hospitalization, such as delirium, pneumonia, and respiratory failure.4,10 Two-thirds of all patients who fall sustain recurrent falls within the next 12 months.6,8
Pathophysiology
Normal physiologic changes in older adults include decreased cardiac output and maximum heart rate, decreased muscular strength and flexibility, decreased pulmonary reserve and oxygen exchange capacity, and decreased bone density.4 These changes are exacerbated by muscle atrophy, deconditioning, gait instability, balance impairment, frailty, sedentary lifestyles, visual impairment, polypharmacy, and numerous medical conditions that place the older adult patient at an even greater risk for falls and injury. (See Table 1.) Older adults have higher rates of arthritic disease and are predisposed for a higher incidence of spinal injuries than similar mechanism counterparts.11 Cerebral atrophy, vascular frailty, hypertension, ubiquitous atherosclerosis, and reduced cerebral autoregulation all increase the risk of intracranial pathology, including subdural hemorrhage and hypoxic brain injury, from a fall.12
Table 1. Physiologic Considerations in Older Adult Fall Patients |
||
Organ System |
Physiology |
Consequence |
Neurologic |
|
|
Musculoskeletal |
|
|
Dermal |
|
|
Hematologic |
|
|
Cardiovascular |
|
|
Pulmonary |
|
|
Hepatorenal |
|
|
Since physiological and chronological age are highly variable in this population, fall patients may not have a generalizable pattern of injury. Not all elders are frail; however, age generally confers frailty in addition to increased comorbidities.4 As age increases, major traumatic injuries may be present with lower mechanisms of injury, such as a fall from the bed to the floor. For example, an octogenarian with a ground-level fall is more likely to sustain cervical spine, upper extremity, pelvic, and rib fractures than a younger elder. Worsening injury severities portend an increased mortality as well.13
Presentation and Initial Evaluation
After a higher mechanism fall, such as a fall from a distance of greater than 20 feet, severe head injury, low GCS score, or obvious deformity of more than two long bones should involve coordination across trauma surgery and critical care specialties, sometimes called “trauma alert.” Although it requires further study, an increased trauma alert level for patients older than 70 years of age has been shown to decrease mortality and hospital length of stay.14 Consider age as a risk factor in itself for increased mortality for similar traumas during triage because the three greatest risk factors for undertriage include being female, falls, and age.9
Diagnostic studies need to evaluate for a broad differential diagnosis in a cost-effective manner and should be guided by the patient’s history and physical exam. Ask about loss of consciousness and duration, witnesses to the fall, seizure-like activity (including tongue biting and loss of bowel or bladder control), alcohol and substance use, comorbid conditions, and medication use. Include questions about provocation, prodrome, and prior history of falling.15 Interview EMS and family members for collateral details. Differentiation between seizure and syncope requires a witnessed account; syncopal falls commonly exhibit brief, unsustained seizure-like activity.15 Prehospital EMS providers can offer critical information on the conditions and environment that elaborate on the presentation, scene construct, and initial vital signs for patients “found down.” Additionally, chart reviews can divulge the patient’s comorbidities, medications, and baseline neurologic status. Finally, do not overlook the review of systems, which adds clues in the search for the cause of a fall.
Physiologic Parameters
When compared to the baseline health of the patient, vital signs predict injury severity and may prompt early recognition of pathology. Be wary of a patient with chronic hypertension and a systolic blood pressure (SBP) of 90 mmHg; reductions in SBP of 30 mmHg below baseline may be hypoperfusing vital organs.4 Review medication lists for antihypertensives, cardiac rate or rhythm control agents, and anticoagulation medications to properly contextualize the vital signs of the older patient in the setting of a trauma resuscitation. Older adult patients are at an increased risk of thermal injuries due to mobility restrictions, physiology, and medications. Work with the nursing team to obtain a core temperature early, and prevent hypothermia with external warming measures. For patients who present with core temperature < 35°C or > 40°C, consider endocrine, infectious, or toxicologic pathology and environmental injury in the differential. In the unstable patient, initiate multiple large bore intravascular access, with intraosseous access as an alternative if vascular access cannot be achieved. Place the patient on the cardiac monitor and continuous pulse oximetry, addressing hypoxia with supplemental oxygen. Begin resuscitation to achieve a mean arterial pressure (MAP) goal of > 65 mmHg.16
Traumatic Evaluation and Management
Advanced Trauma Life Support
In the older adult population, ground-level falls are the most common mechanisms of trauma.5,13 Follow the advanced trauma life support (ATLS) protocol; prioritize the airway, breathing, and circulation in the clinically unstable or unconscious patient.17 Include the extended focused assessment with sonography in trauma (EFAST) in the primary survey to assess for the presence of intra-abdominal free fluid, pericardial effusion, and appropriate bilateral lung sliding. Intervene early and reassess quickly since older adults have less adept physiologic compensation to hypovolemia and shock. Protect the patient from the trauma “triad of death”: hypothermia, acidosis, and coagulopathy, including iatrogenic causes during the resuscitation.18 The ATLS-10, the 2018 update, places emphasis on vital sign trends and base excess to assess hemorrhage class and transfusion needs, instead of using static values.7
Balance the risk of airway compromise with high mortality of intubated older adult patients (20% of those > 80 years of age) when determining if intubation is needed. Hypoxia and hypotension increase complications and mortality for this population during airway management, so adequately plan, preoxygenate, optimize resuscitation, and prepare to manage hemodynamic instability.19 Special procedural considerations for intubation in this population include dentures, limited neck extension, and decreased temporomandibular joint mobility; favorable positioning and video laryngoscopy can assist to overcome these challenges.19 Ensure cervical spine immobility when assessing the airway, if indicated. Regardless of intubation status, assess for symmetrical chest rise with auscultation of breath sounds, and look for hemorrhage while ensuring equal and strong pulses in all extremities.17 Ensure judicious use of small volume boluses of intravenous crystalloid fluid for hypotension since it potentially can worsen coagulopathy and acidosis; initiate blood product resuscitation early for evidence of hemorrhage.17
When evaluating disability, a decreased GCS score may misrepresent neurologic injury if the patient’s baseline is not 15.7 Lastly, remove the patient from the backboard as soon as possible because older individuals have increased risk of skin breakdown in a shorter period of time.4 Complete a secondary survey with a thorough physical exam as well as ancillary imaging of musculoskeletal injury and computed tomography (CT) as indicated.17 Forgo advanced imaging if the patient requires transfer unless it will change management, since a delay in transfer to a higher level of care can be detrimental.7
Pain Management
Appropriately treat severe pain since uncontrolled pain increases the incidence of delirium.20 Achieve pain control through a combination of non-opiate medications with cautiously reduced doses of opiates. Older adult patients have increased sensitivity and increased adverse effects of opiates with hypotension, respiratory depression, and delirium.20,21 Acetaminophen 1,000 mg intravenous (IV) every six hours is a safe option for pain control in the absence of liver failure. If possible, avoid nonsteroidal anti-inflammatory drugs (NSAIDs) because of the potential for medication interactions, renal impairment, and gastric mucosal damage.20 The intubated patient needs to have appropriate sedation with a combination of fentanyl (25 mcg/h to 200 mcg/h), propofol (5 mcg/kg/min up to 4 mg/kg/h), midazolam, and/or dexmedetomidine (0.2 mcg/kg/h to 0.7 mcg/kg/h) to achieve pain control and the Richmond Agitation-Sedation Scale target.16
Intracranial Injury
A primary consideration in the evaluation of older adult falls is traumatic brain injury (TBI). Mortality is directly related to increased age and low GCS score.22 The differential for older adult TBI should encompass cerebral contusions, traumatic subarachnoid hemorrhage, subdural and epidural hemorrhage, skull fracture, facial fractures, and diffuse axonal injury. The risk of injury incurred with anticoagulation use and a low-level fall still is unknown, but warfarin specifically increases the likelihood of mortality.4,22
A noncontrast CT scan of the head is indicated in the evaluation of older adult head injury, since this population experiences increased consequences of similar bleeds than younger patients. Older adult patients may exhibit fewer or later clinical signs of increased intracranial pressure (ICP). A normal GCS score does not prove the absence of clinically significant intracranial injury.12
Subdural hematoma (SDH) is the most common type of hemorrhage.12 SDH can present as deteriorating mental status over several hours, but an estimated 20% to 30% can be caused by arterial bleeding and may present with coma.16 Head CT sensitivity for SDH is close to 100%.16 Also consider a subarachnoid hemorrhage (SAH) as a potential cause of a fall in addition to a sequela of head injury. Detection of SAH with CT exhibits a sensitivity of greater than 99.0% and a specificity 99.9% if it is within six hours of headache onset. For those with symptoms for a longer duration, obtain a CT angiogram or lumbar puncture.23 Dual energy CT is 96% sensitive and 99% specific for intraparenchymal hemorrhage (IPH).24
Declining mental status, pupillary asymmetry, and extensor posturing are signs of cerebral herniation. Rapidly address these findings with measures to lower ICP: Elevate the head of the bed, ensure that a cervical collar does not occlude venous drainage, and cautiously use hyperventilation for brief periods of time to a PaCO2 target of 30 mmHg.12,16 Hyperosmolar therapy can be 3% hypertonic saline or mannitol, at 1 g/kg to 1.5 g/kg boluses.16 In patients with TBI, target SBP >> 100 mmHg in those 50 to 60 years of age, and > 110 mmHg in those older than 70 years of age. Steroids, therapeutic hypothermia, and hyperventilation within the first 24 hours are not recommended.7,16 Tranexamic acid (TXA) has marginal mortality benefit for a hemorrhagic TBI, but may reduce hematoma expansion.25-27 Consider initiating seizure prophylaxis with levetiracetam 500 mg to 1,000 mg orally or IV or phenytoin/fosphenytoin.12,16
Hematologic Considerations
Consider anticoagulation reversal in patients with life-threatening hemorrhage, but especially those with hemodynamic instability or hemorrhage into enclosed spaces. Reversal of anticoagulation and surgical intervention for hemorrhagic complications of head injury are individualized decisions based on the patient’s indication for anticoagulation and risk of continued bleeding weighed against the risk of thrombogenesis.28 Agents for direct oral anticoagulant (DOAC) reversal include idarucizumab, given in a single 5 g IV dose to reverse dabigatran, and andexanet alfa for reversal of the factor Xa inhibitors apixaban and rivaroxaban.28 Ciraparantag is under development for a universal factor for the reversal of Xa and direct thrombin inhibitors.12,28 In those with intracranial hemorrhage (ICH), reverse warfarin with 25 U/kg to 50 U/kg of 4-factor prothrombin complex concentrate (4FPCC, brand names Kcentra or Beriplex P/N) and vitamin K 10 mg IV push, or fresh frozen plasma (FFP) if 4FPCC is not available.16,22 (See Table 2.)
Table 2. Anticoagulation Reversal |
||
Anticoagulant |
Treatment |
Dose |
Aspirin |
Desmopressin |
0.4 mcg/kg |
Vitamin K antagonist: Warfarin |
Vitamin K AND 4-factor prothrombin complex concentrate (4FPCC) OR Fresh frozen plasma (FFP) |
10 mg IV 25 U/kg to 50 U/kg IV 12 mL/kg to 15 mL/kg IV |
Direct thrombin inhibitor: Dabigatran |
Idarucizumab |
5 g IV |
Factor Xa inhibitors: Apixaban, rivaroxaban |
Andexanet alfa |
Low dose: 400 mg IV High dose: 800 mg IV |
Enoxaparin |
Protamine sulfate |
1 mg IV |
Direct thrombin inhibitors Factor Xa inhibitors |
Ciraparantag* |
100 mg to 300 mg IV |
IV: intravenous * In development |
||
There is no reversal for antiplatelet agents that has shown improvement for ICH outcomes.12 Desmopressin does not slow antiplatelet agent-facilitated intracranial hemorrhage and may worsen outcome.29 Transfusion of platelets is recommended only to maintain platelets > 75 × 109/L in the preoperative setting; trending platelet function testing to guide platelet transfusion is not recommended.16 Consult neurosurgery or expeditiously transfer a patient to a facility with neurosurgical capabilities if there is evidence of increased ICP, declining GCS score, focal neurologic deficits or CT evidence of > 5 mm midline shift, SDH with > 10 mm clot thickness, or > 30 cm epidural hematoma volume.12
Spinal Cord Injury
Ground-level falls are the leading cause of spinal cord injury in older adults, the majority of which occur at C1-C4. 13,30,31 Older adult fall patients are twice as likely to have C-spine injuries when compared to younger trauma patients.4 Cervical spine injuries may present with minimal or no neck pain. A diminished level of alertness, distracting injuries, or obvious signs of trauma to the head or neck should prompt clinical suspicion of a C-spine injury.32 Restrict cervical spinal motion until injury is ruled out and complete a thorough neurologic exam, including a cranial nerve and sensory exam. Any neurologic deficits warrant urgent subspecialty consultation.11
The National Emergency X-Radiography Utilization Study (NEXUS) criteria are useful for evaluating use of imaging for low-risk cervical spinal fracture, with 99.6% sensitivity for identification of C-spine injury.32 However, it is recommended that a conservative approach is taken with a low threshold for imaging older adult patients.33 Alternatively, the Canadian C-Spine rule automatically designates adults > 65 years of age as high risk and recommends radiographic imaging.11 CT is the gold standard to identify vertebral fracture or dislocation, with a sensitivity of 98%.11 Plain film X-ray demonstrates a sensitivity of 52% for identification of cervical spine fractures and may be considered if CT is unavailable.11,30 If one spinal fracture is found, CT the entire spinal column because 10% to 40% of patients will have multiple spinal fractures.4,11,30 Obtain MRI for clinical concern of ligamentous, soft tissue, or spinal cord injury, and magnetic resonance angiography (MRA) for concern for vascular injury.11 If spinal cord injury is found, avoid movement that could worsen the injury and optimize tissue perfusion with a MAP goal of 85 mmHg to 90 mmHg, thereby maximizing oxygen delivery.30
Skeletal Injury
The most common injuries sustained in falls include head and hip injuries.6 A history of osteoporosis, chronic kidney disease, or chronic steroid use put the patient at an increased risk for fracture. In addition to a complete evaluation of the extremities and immediate reduction of fractures with neurovascular compromise, palpate the chest wall for tenderness, crepitus, or deformity.7 CT imaging of the chest can show rib fractures as well as underlying lung injury, with a sensitivity and specificity for fractures of 95.5% and 99.9%, respectively, compared to a poor sensitivity of chest X-ray alone.33,34 Point-of-care ultrasound identifies rib fractures as well as pneumothorax and facilitates intervention with nerve blocks, but definitive imaging still may be needed to further delineate management.33
Consult general surgery or trauma surgery if the patient has bicornuate rib fractures or flail chest, since the patient may be a candidate for rib plating. Best in-hospital practices for patients older than 45 years of age with more than two rib fractures include aggressive pain control, pulmonary toilet, and prophylactic noninvasive ventilation (NIV) in attempts to reduce intubation and intensive care unit (ICU) admission during hospitalization.35 For ED management, attempt pain control and NIV before immediate intubation in appropriate candidates who present with respiratory distress secondary to rib fractures. Ultrasound-guided serratus plane block performed by the emergency physician also can bolster pain control. In addition to cardiac monitoring, intralipid rescue should be at the bedside for all plane and nerve blocks with potential for toxicity. Use a long 22-gauge needle to place 20 mL to 40 mL of anesthetic, typically 0.25% bupivacaine or 0.5% ropivacaine diluted in a larger volume, between the external intercostal ribs and serratus anterior muscle centered along the fractured ribs.36 For older adult patients or those with renal or liver disease, use 20% less anesthetic.36 The anesthetic bathes the lateral cutaneous branches of the intercostal nerves and then the intercostal nerves to achieve a multi-level block. Direct visualization with ultrasonography reduces the risk of pleural disruption during fascial layer infiltration.37
Isolated non-displaced rib fractures without underlying pulmonary pathology may be considered for discharge with appropriate pain control and return precautions. Otherwise, have a low threshold to hospitalize an older adult with rib fractures for pain management and observation.3 Risk factors for the development of pneumonia in these patients include more numerary fractures, male gender, alcohol use, and higher volumes of initial IV fluids.23
Falls are a significant mechanism for femur fractures in older adults, most commonly femoral neck and intertrochanteric fractures. Physical exam findings may include leg shortening, external rotation, severe pain to hip manipulation, and the inability to bear weight. Patients may complain of groin pain or knee pain, since these are common sites of referred pain.
Complete an evaluation of the femoral nerves with motor and sensory testing. X-rays are 90% to 98% sensitive for hip fractures, but occult fractures are best diagnosed by MRI if X-ray is nondiagnostic and pain continues. Evaluate pelvic X-rays for both Shenton line and neck-shaft angle within 120-130 degrees. (See Figure 1.)
Figure 1. Left Intertrochanteric Fracture with Shenton Line Demonstrated on the Right Side |
 |
Image used with permission from Catherine Marco, MD, Wright State University Emergency Medicine |
Hemorrhage can be significant with intertrochanteric and subtrochanteric fractures; have a low threshold for blood product resuscitation. The most common complications during hospitalization after a hip fracture include venous thromboembolism and pulmonary infection, but femoral neck fractures can lead to avascular necrosis due to a risk for disruption of the medial and lateral femoral circumflex arteries.38 Consult anesthesia and orthopedic specialists because the best management is multidisciplinary with early surgical correction. Optimize the patient for surgery, including management of electrolyte imbalances and comorbid conditions.39 Fascia iliaca block has been shown to improve patient outcomes with fewer side effects than opiates.21
Other fractures also are sustained in falls. The incidence of ankle, clavicle, hand, and humerus fractures continues to increase, especially in the older female population.40 Examine these regions well and, as with all fractures, verify distal neurovascular function and reassess after every patient transfer, repositioning, or splinting procedure.
Medical Evaluation and Management
After the initial trauma evaluation, stabilization, and appropriate specialty consultation, conduct a thorough medical investigation for the cause of falls in an older adult patient tailored to the patient’s history of present illness and comorbidities. Obtain a point-of-care glucose level.41 The electrocardiogram (ECG) can provide a wealth of information, such as electrolyte abnormalities and toxicologic patterns. Look for ischemia, dysrhythmia, interval abnormalities such as long QT or short PR, hypertrophic cardiomyopathy, Brugada syndrome, arrhythmogenic right ventricular cardiomyopathy, or atrial septal defect.15,42 Further diagnostic testing is presentation driven.43
Syncope
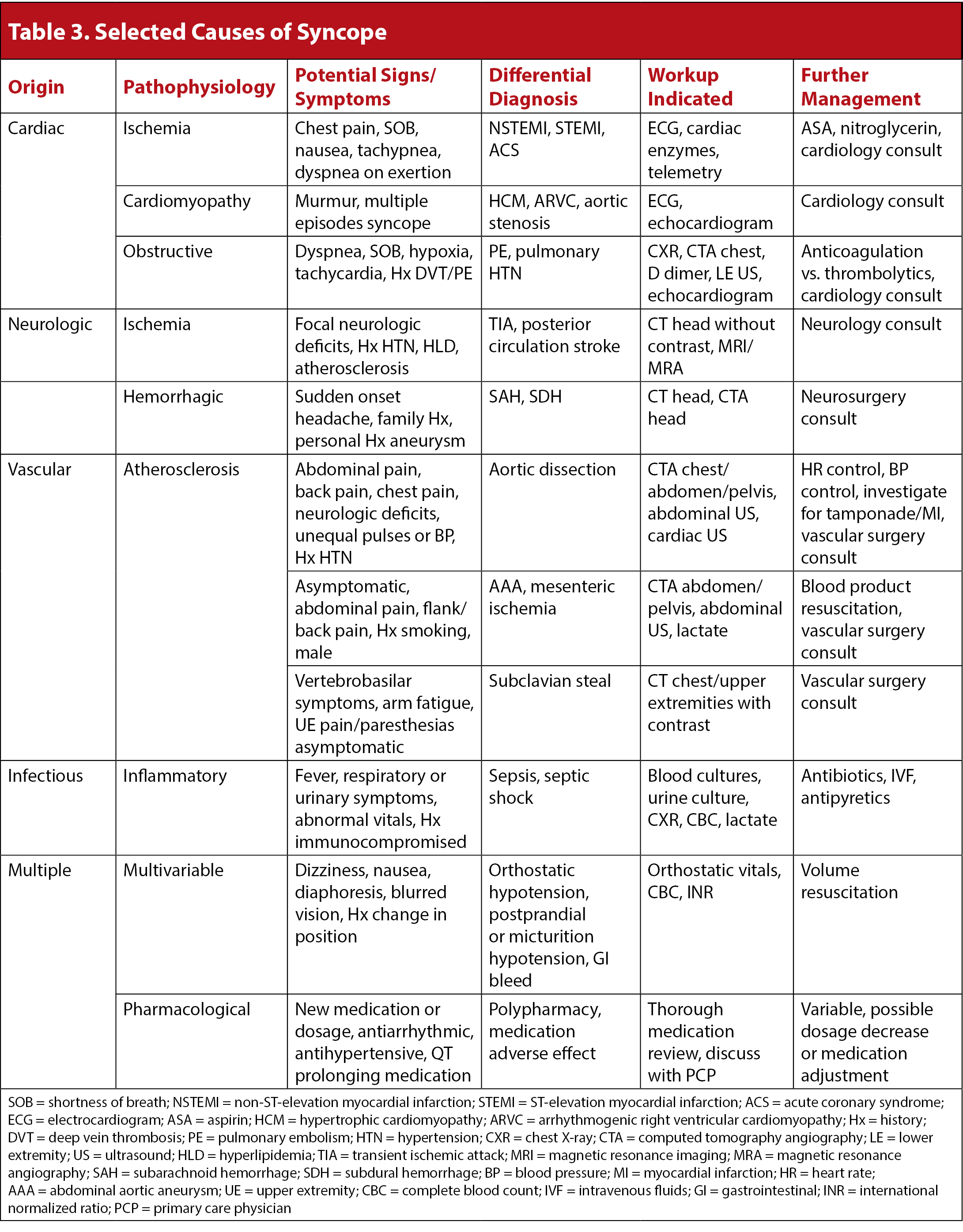
Older adults have an increased incidence of syncope starting at age 70 years.44 Consider syncope in unwitnessed falls, facial trauma, or falls in cognitively impaired patients who cannot accurately recall the events.44 The most clinically concerning causes of syncope are cardiogenic and neurologic, while the most common causes of syncope are orthostatic or postprandial hypotension, cardiogenic, vasovagal, and neurologic.44, 45 Cardiac causes of syncope have a high mortality rate, about 10% in six months, and underlying cardiac pathology increases this risk.44,45 (See Table 3.)
The most important initial components in the evaluation of syncope include history, physical exam, and ECG. Consider structural abnormalities such as myocardial hypertrophy or ischemia, pulmonary embolism (PE) or pulmonary hypertension, and valvular pathology, especially aortic stenosis. Older adult patients have less physiologic reserve to maintain cerebral perfusion in the event of decreased cardiac output due to dysrhythmias. Treat ongoing dysrhythmias according to the advanced cardiac life support (ACLS) protocol. Patients with conduction abnormalities, such as bundle branch blocks and fascicular blocks, even if chronic, carry a higher mortality than patients without ECG abnormalities.45 Obstructive PE in patients with dyspnea, tachypnea, or chest pain, especially in those with a history of venous embolism or malignancy, is best investigated with CT angiogram of the chest, with a sensitivity of 92.9% and a specificity 85.7%, compared to a V/Q scan, which has a sensitivity of 57.1% and specificity of 47.8%.43,46 Carotid massage to diagnose carotid sinus syndrome, which is a less common cause of older adult syncope, can be a high-risk maneuver without a high diagnostic yield; it generally is not performed.44,47
Anemia may cause a lightheaded sensation, shortness of breath, or generalized weakness. Evaluate for a gastrointestinal (GI) bleed with a fecal occult blood test in patients with a history of previous GI bleeding or melena, frequent or routine NSAID use, abdominal pain, anticoagulation medication use, or anemia on complete blood count.41
Monitor continuous telemetry and oxygen saturation, with bilateral upper extremity blood pressures to evaluate for aortic dissection or subclavian steal. Consider subclavian steal when syncope, upper extremity fatigue, or vestibulobasilar symptoms are reported together.43 Abdominal aortic aneurysm is more common in older adult men who have a smoking history, and carotid or vertebral dissection can be an atypical presentation of stroke-like symptoms.43 Psychiatric causes of syncope are diagnoses of exclusion. Evaluate life-threatening causes first, and hesitate to make these diagnoses in the ED.45
Within the emergency medicine community, some controversy stems from the debate about disposition for patients with syncope. Up to 50% of patients may not have a specific delineation of syncopal pattern in the ED; of the remaining patients who are diagnosed during hospitalization, 80% of the time the culprit pattern is diagnosed in the ED.15,42 Stratify patients into low-, medium-, and high-risk categories and ensure a safe disposition for each.41 Admit high-risk patients with significant cardiac risk factors, including those with a history of structural abnormalities, syncope at rest, exertional syncope, chest discomfort, palpitations, or ECG changes.15,41 For those without definitive risk stratification, several rules can be applied. The San Francisco Syncope Rule is the most studied prediction rule for syncopal outcomes, although validation studies remain inconsistent, and it should augment clinical decision-making.48 Serious adverse events occur for patients with a history of congestive heart failure, hematocrit < 30%, shortness of breath, SBP < 90 mmHg, or ECG abnormalities. Lower-risk features that may support outpatient management in lieu of hospitalization include patients with a long history of similar syncopal events and those with prodromal symptoms typical of reflex syncope: syncope after prolonged standing in warm environments, postprandial syncope, or syncope triggered by cough, urination, defecation, or positional changes.15,41
Alternatively, the Canadian Syncope Rule aims to assess and predict 30-day mortality in patients of all ages with syncope.49 If all factors are negative in the patient who does not have a diagnosed cause of syncope, less than 2% of patients followed in the study sustained a serious outcome.48
Consider admitting patients with a score of 1 or higher on the Canadian Syncope Rule.49 Intermediate-risk patients should be monitored on ED telemetry for at least three hours. Admit patients for further workup in the event of a pause greater than three seconds, ventricular tachycardia, high-grade AV block, or bradycardia.41 Counsel patients to avoid high-risk activities, such as driving, until cleared at a follow-up reassessment. For a list of syncope causes discussed, see Table 3.
Iatrogenic
Patients taking multiple medications should have a review for interactions.41 Anticoagulation, even with clopidogrel, may increase the length of stay in the hospital.50 There is growing evidence that anticoagulation may present less of a risk factor than previously thought for the development of ICH; however, a conservative approach with a low threshold for imaging may prevent significant morbidity for patients on anticoagulation.22,51 Beta-blocker and/or calcium channel blocker use may blunt tachycardic response and decrease recognition of clinical instability.4 Medications with arrhythmogenic, QT alteration, or antihypertensive properties should be taken into consideration as a potential cause of syncope.41,45 Include over-the-counter medications and supplements during the review of medications for polypharmacy, defined as five or more medications.44,52 The association between polypharmacy, increased gait disturbance, and prevalence of falls is well established, even when corrected for age, comorbidities, and gender. It also is important to consider that each medication added to an older adult with polypharmacy increases the person’s likelihood of a fall.52
Neurologic
Differentiate syncopal falls, which exhibit rapid onset, short duration, and complete resolution without medical intervention, from falls secondary to neurologic pathology. Fall risk is greater for patients with chronic neurologic disorders, such as stroke or dementia; combined disorders convey even greater risk than each disorder alone.53 Screen for stroke mimics by asking about a history of depression or psychiatric illness, epilepsy, migraine, and comorbidities, such as hypertension, diabetes, and atrial fibrillation.54 There is no validated scoring tool to rule out stroke mimics in ED patients.54
Focal neurologic deficits or an elevated National Institutes of Health Stroke Scale (NIHSS) score warrant immediate neurologic specialty consultation, with particular urgency if the symptoms onset within the window for tissue plasminogen activator (tPA) treatment. Optimize blood pressure to SBP < 180 mmHg and diastolic < 110 mmHg in candidates for tPA.55 Trauma is not an absolute contraindication to tPA, but it requires a clear discussion and shared clinical decision-making with the patient who may be at increased risk for subsequent bleeding. Review home medication lists with pharmacy for interactions to tPA. The American Academy of Emergency Medicine clinical practice guidelines have not found any evidence to reduce ambiguity for emergency medicine physicians regarding the use of tPA in patients older than 80 years of age or for time windows > 4.5 hours. However, evidence exists for improved morbidity and mortality with admission to a specified stroke unit.56 Emergent neurosurgical interventions with thrombectomy use eligibility criteria and especially seek to include internal carotid artery/middle cerebral artery-sphenoidal segment of MCA (ICA/MCA-M1) occlusion of less than six hours duration, with an NIHSS score ≥ 6 and large vessel occlusions in anterior circulation.57 The NIHSS has decreased detection for posterior circulation ischemia and, similarly, a noncontrast head CT only has a sensitivity in up to 49% of cases for cerebellar pathologies.58,59 Consider posterior stroke in the fall patient with acute onset dizziness with persistent symptoms, altered mental status, dysarthria, neck pain, nausea and/or vomiting, and weakness.60 The head-impulse, nystagmus, test of skew (HINTS) exam is 96% to 100% sensitive for posterior stroke. Apply it to patients with persistent dizziness without C-spine pathology.60
Transient ischemic attack (TIA) also mimics stroke and may precipitate falls; it is defined as tissue ischemia without evidence of infarct. The American College of Emergency Physicians (ACEP) clinical policy no longer recommends the ABCD2 score as a sole risk-assessment for a patient’s likelihood to have short-term strokes after a TIA. MRA and cervical vascular imaging, including carotid ultrasound, are useful to predict short-term strokes in patients with suspected TIA. Rapid diagnostic protocols to assess 30-day stroke risk for ED patients may decrease cost and length of stay, and can be performed if high-risk features are absent: abnormal head CT, suspected embolic source, known carotid stenosis, history of large stroke, or crescendo TIA.61
A fall with seizure-like activity should raise suspicion for severe electrolyte abnormalities such as hyponatremia or hypoglycemia, or intracranial pathology such as a mass or hemorrhage. Lateral tongue biting and a post-ictal phase suggest a seizure, although incontinence or tonic-clonic movements are not necessarily specific.41,43 Check medication levels of patients with known seizures if they are taking medications with available assays. Evaluate for meningeal signs and fever as a cause of seizure. Evaluate a creatinine kinase (CK) to identify the diagnosis of rhabdomyolysis secondary to unwitnessed seizure activity, prolonged immobility, or compartment syndrome. Examine all extremities thoroughly for compressive injuries, particularly in the anticoagulated patient. For CK elevated above five times the upper limit of normal, manage the patient with hydration, electrolyte evaluation and correction, and monitoring of renal function and urinary output. Consider metabolic derangements as the cause of altered mental status without focal deficits, such as hypertensive encephalopathy, uremic encephalopathy, hyperammonemia, thyroid storm or thyrotoxicosis, and myxedema coma.
Infectious
Older adult patients may not mount a fever or leukocytosis as a clue for sepsis.41 Evaluate for systemic inflammatory response syndrome (SIRS) criteria, including heart rate > 90 beats per minute, temperature < 36°C or > 38°C, respiratory rate > 20 breaths per minute, PaCO2 < 32 mmHg, white blood cell count < 4 × 109 cells/L or > 12 × 109 cells/L, and immature bands > 10%. Ask about preceding infectious symptoms, such as respiratory illness, urinary symptoms, and fever, chills, or malaise in all fall patients. Urinary tract infections and lower respiratory tract infections are the most commonly found infectious sources in fall patients.62,63 Examine the patient’s skin, since cellulitis may go unnoticed. If infection is suspected, collect blood cultures to ensure proper coverage and length of treatment for admitted patients. Lactic acidemia, a nonspecific estimate of decreased tissue perfusion, can be associated with infection and may serve as a laboratory marker of resuscitation for inpatient providers. Follow Surviving Sepsis guidelines to include hemodynamic resuscitation and early antimicrobials to cover likely pathogens.64 Use norepinephrine as the initial agent and add vasopressin if the target MAP goal of > 65 mmHg is not achieved.65 Central venous pressure is no longer recommended as a sole hemodynamic evaluation monitor, so use multiple dynamic monitors.64
Special Populations
There is a four-fold increase of falls in dialysis patients compared to their age-matched peers.66 Half of dialysis patients are older than 65 years of age.66 Hemodialysis patients have protein wasting leading to malnutrition, decreased bone density, chronic inflammation, cognitive decline, and reduced physical capabilities due to decreased muscle mass and fitness.66,67 Maintain a high clinical suspicion for fractures in this population, even with low mechanisms of injury. Dialysis patients also have a higher incidence of polypharmacy, compounding their increased risk.66
Chronic alcohol use in older adult patients can contribute to even greater risks of trauma from falls through increased cerebral volume loss, coagulopathies through liver disease, and an overall weaker immune system. Alcohol use has been found to be associated with an increased severity of injury in older adult outdoor falls.68 IV substance abuse increases the patient’s risk for bloodborne pathogens of hepatitis B, hepatitis C, or human immunodeficiency virus, which complicate medical and trauma management. Substance abuse is expected to increase among the older adult population in the next decade. Older adult trauma patients should be screened for alcohol and substance use to determine the potential benefit of social work or behavioral health interventions in this currently underevaluated population.69
Special Considerations and Controversies
Cost
Healthcare costs exceed the gross domestic product growth per capita in the United States, a trend that is expected to continue.70 Falls in older adults add to the already burdened global healthcare system.8 Efficient use of evaluation tools can assist in judicious medically appropriate management. A urinalysis is relatively inexpensive (about $20 to $26 cash price without insurance), but the national average cash price of a chest X-ray for patients without insurance is $280.71,72 CTs represent the highest cost and the area for greatest improvement. For example, abdominal solid organ injuries after a fall in an older adult are found in < 1% of patients, and even fewer warrant surgical intervention.5,13 A CT evaluation of a low-impact fall for occult intra-abdominal injuries likely has a low clinical yield for patients with a reassuringly negative physical exam as well as a negative focused assessment with sonography for trauma (FAST) exam.5
As another example, head CT evaluations in older adult patients represent a potential for process improvement. Older adults at baseline mental status with low-risk falls without loss of consciousness or signs of head trauma may not need a head CT.73 However, this is a controversial topic. Older adult patients who present from a noninstitutional setting or who demonstrate signs of head trauma are at an increased risk for ICH, even in the absence of focal neurologic findings.52 The Canadian CT Head Rule emphasizes age ≥ 65 years or anticoagulation use as risk factors for major head injury. Conversely, the New Orleans Criteria indicate a head CT for head injury patients with risk stratification based on age > 60 years and loss of consciousness. Balance the cost of a head CT, between $211 and $2,200 depending on location, with the patient’s risks.74
Abuse
Older adult patients are particularly vulnerable to caregiver abuse, including injury and neglect. Nonaccidental trauma and neglect should be considerations for injuries in older adults. Head, neck, and face trauma are the most common areas of injury in elder physical abuse.75 For example, traumatic hair pulling may lead to subgaleal hematoma, which is easily mistaken for a head injury from a fall.75 Maxillofacial and extremity bruising should be evaluated for various stages of healing and the shape of hands or objects. First responders provide additional information about the patient’s living situation and details of the story that an altered or injured elder may not be able to supply.76 Complete a physical exam for other signs of neglect, such as skin ulcerations and poor hygiene. Elder neglect is the most common cause of elder abuse.77 Do not assume that malnutrition and dehydration are the results of self-neglect in a debilitated patient. Several risk factors for elder abuse include financial dependence of the caregiver upon the elder, or substance abuse by the caregiver.75 Contact adult protective services if abuse is suspected and understand the reporting laws in your state.76
Disposition
Disposition needs to be carefully considered in the older adult with a fall, driven by diagnosis and, most importantly, the patient’s goals of care. Respect patient autonomy: When the information is available, follow the patient’s living will. Be familiar with local state laws about do-not-resuscitate orders, living wills, and power of attorney. It is the physician’s responsibility to provide counsel and psychosocial support, and to present all treatment options to their patients. Consider safety, ability to obtain follow-up, transportation issues, caregiver limitations, and the possibility of elder abuse.
Outcomes studied in both medical and surgical admissions of ground-level fall blunt traumas at a single center showed no difference in survival when adjusted for comorbidities and trauma injury severity score, so an admission to the most appropriate service is warranted according to local practices.3 Admit to the ICU for hemodynamic instability, polytrauma, intracranial trauma, or comorbidities that need to be managed closely. Discharge can be considered in those without significant traumatic injury, a discovered and benign cause of falling, and access to adequate follow-up. The Eastern Association for the Surgery of Trauma guidelines recommend that patients > 65 years of age with comorbid conditions or severe anatomic injuries be transferred to trauma centers because they have a higher tendency to require specialty care.14 Older adult patients would benefit from referral to multidisciplinary providers if possible within the community, including evaluation referrals for vision, hearing, and cognitive functioning as well as a home safety assessment. Counsel patients about fall prevention, including transfer safety and environmental safety for tripping or slipping hazards, and involve family/caregivers in the discussion if possible.8
Summary
Older adults are the fastest growing patient population in trauma.3 Falls in patients older than 65 years of age are an increasingly common presentation in U.S. EDs, and intricate knowledge and confidence in the evaluation and management of these patients is vital. Older adult patients are complex because of their physiologic differences and comorbidities in addition to higher morbidity and mortality after low-level trauma. Disposition must be considered not only for the patient, but also for their caregivers or family members.
REFERENCES
- Centers for Disease Control and Prevention. Older adult fall prevention. May 9, 2024. https://www.cdc.gov/falls/data-research/facts-stats/
- Burns ER, et al. The direct costs of fatal and non-fatal falls among older adults — United States. J Safety Res 2016;58:99-103.
- Barry RG, et al. Comparison of geriatric trauma outcomes when admitted to a medical or surgical service after a fall. J Surg Res 2019;233:391-396.
- Fleischman RJ, Ma OJ. Trauma in the elderly. In: Tintinalli JE, et al, eds. Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw Hill; 2016:1688-1692.
- Gartin CG, et al. Injury patterns and incidence of intra-abdominal injuries in elderly ground level fall patients: Is the PAN-SCAN warranted? Am J Surg 2019;218:847-850.
- Galet C, et al. Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: A query of the WHO mortality database and National Readmission Database from 2010 to 2014. Clin Epidemiol 2018;10:1627-1637.
- Galvagno SM, et al. Advanced Trauma Life Support Update 2019: Management and applications for adults and special populations. Anesthesiol Clin 2019;37:13-32.
- Vieira ER, et al. Prevention of falls in older people living in the community. BMJ 2016;353:i1419.
- Hartholt KA, et al. Mortality from falls among US adults aged 75 years or older, 2000-2016. JAMA 2019;321:2131-2133.
- de Vries R, et al. Older polytrauma: Mortality and complications. Injury 2019;50:1440-1447.
- Kanwar R, et al. Emergency department evaluation and treatment of cervical spine injuries. Emerg Med Clin North Am 2015;33:241-282.
- Beedham W, et al. Head injury in the elderly — an overview for the physician. Clin Med (Lond) 2019;19:177-184.
- Bhattacharya B, et al. The older they are the harder they fall: Injury patterns and outcomes by age after ground level falls. Injury 2016;47:1955-1959.
- Carr BW, et al. Increased trauma activation is not equally beneficial for all elderly trauma patients. J Trauma Acute Care Surg 2018;85:598-602.
- Reed MJ. Approach to syncope in the emergency department. Emerg Med J 2017;36:108-116.
- Al-Mufti F, Mayer SA. Neurocritical care of acute subdural hemorrhage. Neurosurg Clin N Am 2017;28:267-278.
- ATLS Subcommittee; American College of Surgeons’ Committee on Trauma; International ATLS working group. Advanced trauma life support (ATLS): The ninth edition. J Trauma Acute Care Surg 2013;74:1363-1366.
- Murphy P, et al. Understand the trauma triad of death. EMS World. February 2012. https://www.emsworld.com/article/10565011/understand-trauma-triad-death
- Theodosiou CA, et al. Rapid sequence induction of anaesthesia in elderly patients in the emergency department. Resuscitation 2011;82:881-885.
- Tsang KS, et al. Can intravenous paracetamol reduce opioid use in preoperative hip fracture patients? Orthopedics 2013;36(Suppl 2):20-24.
- Falyar C, Tola D. Ultrasound-guided fascia iliaca blocks in the emergency department. Geriatr Nurs 2019;40:441-444.
- Batey M, et al. Direct oral anticoagulants do not worsen traumatic brain injury after low-level falls in the elderly. Surgery 2018;164:814-819.
- Marco CA, et al. Risk factors for pneumonia following rib fractures. Am J Emerg Med 2019;Nov 18. doi:10.1016/j.ajem.2019.10.021.
- Hu R, et al. Dual-energy head CT enables accurate distinction of intraparenchymal hemorrhage from calcification in emergency department patients. Radiology 2016;280:177-183.
- Sarhan RM, et al. Tranexamic acid in patients with traumatic brain injury: A meta-analysis. Rev Esp Anestesiol Reanim (Engl Ed) 2024;71:360-367.
- Song JX, et al. Therapeutic efficacy of tranexamic acid on traumatic brain injury: A systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 2024;32:18.
- Zhang M, Liu T. Efficacy and safety of tranexamic acid in acute traumatic brain injury: A meta-analysis of randomized controlled trials. Am J Emerg Med 2024;80:35-43.
- Goldin M, et al. Reversal of anticoagulation: Therapeutic advances and clinical guidelines. Am J Therapeutics 2018;25:e44-e52.
- Shahzad F, et al. Safety and efficacy of desmopressin (DDAVP) in preventing hematoma expansion in intracranial hemorrhage associated with antiplatelet drugs use: A systematic review and metaanalysis. Brain Behav 2024;14:e3540.
- Kebaish KM, Harris A. Spine and spinal cord injuries. In: Cameron JL, Cameron AM. Current Surgical Therapy. 13th ed. Elsevier; 2020:1221-1226.
- Hall S, et al. Spinal fractures incurred by a fall from standing height. Clin Neurol Neurosurg 2019;177:106-113.
- Evans D, et al. Application of National Emergency X-Ray Utilizations Study low-risk c-spine criteria in high-risk geriatric falls. Am J Emerg Med 2015;33:1184-1187.
- Alkadhi H, et al. Accuracy and time efficiency for the detection of thoracic cage fractures: Volume rendering compared with transverse computed tomography images. J Comput Assist Tomogr 2004;28:378-385.
- Karlson KA, French A. Initial evaluation and management of rib fractures. UpToDate. Last updated May 21, 2024. https://www.uptodate.com/contents/initial-evaluation-and-management-of-rib-fractures
- Kelley KM, et al. Early use of a chest trauma protocol in elderly patients with rib fractures improves pulmonary outcomes. Am Surg 2019;85:288-291.
- Highland Department of Emergency Medicine, Alameda Health System. Serratus plane block for rib fractures. http://highlandultrasound.com/rib-fractures
- Durant E, et al. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med 2017;35:197.e3-197.e6.
- Steele M, Stubbs AM. Hip and femur injuries. In: Tintinalli JE, et al, eds. Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw Hill; 2016:1842-1849.
- Swift C, et al. Interdisciplinary management of hip fracture. Clin Med (Lond) 2016;16:541-544.
- Court-Brown CM, et al. Fractures in older adults. A view of the future? Injury 2018;49:2161-2166.
- Ali NJ, Grossman SA. Geriatric syncope and cardiovascular risk in the emergency department. J Emerg Med 2017;52:438-448.
- Mattu A, Swaminathan A. Cardiology Corner: Syncope. EM:RAP. Nov. 1, 2019. https://www.emrap.org/episode/emrap20198/cardiology
- Long B, Koyfman A. Vascular causes of syncope: An emergency medicine review. J Emerg Med 2017;53:322-332.
- de Ruiter SC, et al. Multiple causes of syncope in the elderly: Diagnostic outcomes of a Dutch multidisciplinary syncope pathway. Europace 2018;20:867-872.
- Quinn J. Syncope. In: Tintinalli JE, et al, eds. Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw Hill; 2016:380-388.
- Katsouda E, et al. Evaluation of spiral computed tomography versus ventilation/perfusion scanning in patients clinically suspected of pulmonary embolism. In Vivo 2005;19:873-878.
- Wu TC, et al. Carotid sinus massage in syncope evaluation: A nonspecific and dubious diagnostic method. Arq Bras Cardiol 2018;111:84-91.
- Saccilotto RT, et al. San Francisco Syncope Rule to predict short-term serious outcomes: A systematic review. CMAJ 2011;183:E1116-1126.
- Thiruganasambandamoorthy V, et al. Development of the Canadian Syncope Risk Score to predict serious adverse events after emergency department assessment of syncope. CMAJ 2016;188:E289-E298.
- Gurley KL, Edlow JA. Avoiding misdiagnosis in patients with posterior circulation ischemia: A narrative review. Acad Emerg Med J 2019;26:1273-1284.
- Marcolini E, Swaminathan A. Posterior circulation strokes. EM:RAP. Nov. 1, 2019. https://www.emrap.org/episode/emrap20198/posterior
- American College of Emergency Physicians Clinical Policies Subcommittee on Suspected Transient Ischemic Attack; Lo BM, et al. Clinical Policy: Critical issues in the evaluation of adult patients with suspected transient ischemic attack in the emergency department. Ann Emerg Med 2016;68:354-370.
- Coleman J, et al. The effect of anticoagulation status on geriatric fall trauma patients. Am J Surg 2016;212:1237-1242.
- Gangavati AS, et al. Prevalence and characteristics of traumatic intracranial hemorrhage in elderly fallers presenting to the emergency department without focal findings. J Am Geriatr Soc 2009;57:1470-1474.
- Montero-Odasso M, et al. Polypharmacy, gait performance, and falls in community-dwelling older adults. Results from the Gait and Brain Study. J Am Geriatr Soc 2019;67:1182-1188.
- Whitney DG, et al. Fall risk in stroke survivors: Effects of stroke plus dementia and reduced motor functional capacity. J Neurol Sci 2019;401:95-100.
- Khan NI, et al. Novel algorithm to help identify stroke mimics. J Stroke Cerebrovasc Dis 2018;27:703-708.
- Hughes RE, et al. TPA therapy. In: StatPearls [Internet]. StatPearls Publishing. July 4, 2023.
- Meurer WJ, et al. Intravenous Recombinant tissue plasminogen activator and ischemic stroke: Focused update of 2010 clinical practice advisory from the American Academy of Emergency Medicine. J Emerg Med 2018;54:723-730.
- Ren Z, et al. Indications for mechanical thrombectomy — Too wide or too narrow? World Neurosurg 2019;127:492-499.
- Yamada S, et al. DEFENSIVE Stroke Scale: Novel diagnostic tool for predicting posterior circulation infarction in the emergency department. J Stroke Cerebrovasc Dis 2019;28:1561-1570.
- Shu A, et al. Elderly fall patients need a urinalysis. Am Surg 2018;84:299-301.
- Blair A, Manian FA. Coexisting systemic infections in patients who present with a fall. Am J Med Sci 2017;353:22-26.
- Rhodes A, et al. Surviving Sepsis Campaign: International guidelines for management of sepsis and septic shock: 2016. Crit Care Med 2017;45:486-552.
- Guarino M, et al. 2023 Update on Sepsis and Septic Shock in Adult Patients: Management in the emergency department. J Clin Med 2023;12:3188.
- Bhattarai M. Geriatric issues in older dialysis patients. RI Med J 2016;99:15-18.
- Kono K, et al. Development and validation of a fall risk assessment index for dialysis patients. Clin Exp Nephrol 2018;22:167-172.
- Jung HY, et al. Relating factors to severe injury from outdoor falls in older people. Geriatr Gerontol Int 2018;18:80-87.
- Lank PM, Crandall ML. Outcomes for older trauma patients in the emergency department screening positive for alcohol, cocaine, or marijuana use. Am J Drug Alcohol Abuse 2014;40:118-124.
- Jacobs P, et al. Raising the age of eligibility for medicare to 67: An updated estimate of the budgetary effects. Congressional Budget Office 2013;1-5.
- Sidecar Health. Cost of urinalysis by state. https://cost.sidecarhealth.com/c/urinalysis-cost
- Madison B. How much does an X-ray cost? GoodRx Health. Published Nov 27, 2023. https://www.goodrx.com/health-topic/diagnostics/how-much-do-x-rays-cost
- Jeanmonod R, et al. History and physical exam predictors of intracranial injury in the elderly fall patient: A prospective multicenter study. Am J Emerg Med 2019;37:1470-1475.
- Paul AB, et al. How much is that head CT? Price transparency and variability in radiology. J Am Coll Radiol 2015;12:453-457.
- Gibbs LM. Understanding the medical markers of elder abuse and neglect: Physical examination findings. Clin Geriatr Med 2014;30:687-712.
- Carney A. Indicators of abuse in the elderly ICU patient. Crit Care Nurs Q 2015;38:293-297.
- Glauser J, Hustey FM. Abuse of the elderly and impaired. In: Tintinalli JE, et al, eds. Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw Hill; 2016:1991-1996.
Falls cause significant morbidity and mortality among older adult patients compared to younger patients. When treating a patient who has fallen, the emergency medicine physician should identify traumatic injuries and evaluate for medical pathology contributing to the fall, as well as manage the patient.
Subscribe Now for Access
You have reached your article limit for the month. We hope you found our articles both enjoyable and insightful. For information on new subscriptions, product trials, alternative billing arrangements or group and site discounts please call 800-688-2421. We look forward to having you as a long-term member of the Relias Media community.
