Identifying Pediatric Cervical Spine Injuries
Authors
Joy Hallmark, MD, Department of Emergency Medicine, University of North Carolina, Chapel Hill
Daniel Robinson, MD, Department of Orthopedic Surgery, University of North Carolina, Chapel Hill
Daniel Migliaccio, MD, Clinical Assistant Professor, Ultrasound Fellowship Director, Department of Emergency Medicine, University of North Carolina, Chapel Hill
Peer Reviewer
Katherine Baranowski, MD, FAAP, FACEP, Chief, Division of Pediatric Emergency Medicine, Department of Emergency Medicine, New Jersey Medical School, Rutgers, The State University of New Jersey
Executive Summary
- Upper cervical spine injuries (C1-C4) are almost twice as common as lower cervical spine injuries (C5-C7), secondary to the larger head size of children relative to their body, which shifts their fulcrum to the C2/C3 level.
- The Canadian C-spine Rule included no patients younger than 16 years of age. Meanwhile, the National Emergency X-radiography Utilization Study criteria only included 2.5% of patients 8 years of age or younger, and among patients with a cervical spine injury, only 1.3% were 8 years of age or younger.
- Thus, conventional X-rays are the most frequently used initial imaging modality if a very high suspicion for cervical spine injury is not present.
- Computed tomography (CT) scans typically are reserved for patients who have experienced polytrauma, are obtunded, or are at a high risk because of the mechanism of injury or individual risk factors.
- Magnetic resonance imaging (MRI) is the most sensitive and specific imaging modality for acute pediatric spine injury, identifying soft tissue and ligamentous injuries very well, which are poorly visualized on CT scan.
- The basion-dens interval and the interspinous ratio have been shown to have the highest sensitivity and specificity for detecting Atlanto-occipital dissociation and triggering the need for MRI.
- In the setting of trauma, atlantoaxial (AA) instability can be evaluated on lateral cervical spine films, like atlanto-occipital dissociation. The atlas-dens interval (ADI) is measured from the posterior aspect of the anterior ring of C1 to the anterior aspect of the dens. In a pediatric patient, a normal ADI should be 5 mm or less (as opposed to ≤ 3 mm that is considered normal in adults). If the ADI is < 5 mm, it is likely the tectorial membrane is intact. If the ADI is > 5mm in flexion or neutral, or > 4 mm in extension, an MRI should be ordered to further evaluate the ligamentous stabilizing structures.
- An anatomic variant that must be recognized in the pediatric cervical spine is pseudosubluxation. This normal variant can be mistaken for an unstable cervical spine injury if seen on imaging following a trauma. The posterior cervical line is used to distinguish pseudosubluxation from an unstable injury. The posterior cervical line runs along the anterior aspect of the spinous processes on lateral cervical spine films. This line should be within 1 mm of each spinous process on flexion and extension. The posterior cervical line should be smooth and continuous without a sudden step-off or break.
Cervical trauma in pediatrics is fortunately uncommon, but associated with significant morbidity. Early recognition and timely management are essential to optimize the child's outcome. Balanced against this is the need to minimize unnecessary radiation in young children. The authors comprehensively review identifying pediatric cervical spine injuries.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
Introduction and Epidemiology
Cervical spine trauma in children is rare and occurs in only 1% to 2% of blunt pediatric trauma patients. However, out of all pediatric spinal injuries, the cervical spine is the most common level to be affected (60% to 80%) with boys twice as likely to be affected as girls.1,2 Although incidence is low, a high index of suspicion is needed for these injuries because of their significant morbidity. Evaluation poses a unique challenge because of anatomic differences and the difficulty of obtaining reliable physical exams. Additionally, computed tomography (CT) scans are used more judiciously in the pediatric population, given the risk of radiation, so other imaging modalities must be considered.
In young infants and toddlers, the most common mechanisms of injury are falls and high-speed motor vehicle collisions with inappropriate restraint. School-age children and adolescents are at risk for sport and recreational activity-related injuries to the cervical spine, from activities such as diving, football, hockey, cheerleading, and gymnastics, in addition to bicycling/dirt-biking with subsequent crashes.3 Unfortunately, nonaccidental trauma also is a mechanism of injury, although this is less frequent.
It is imperative to have a high index of suspicion for these injuries. The emergency physician should take a thorough history focusing on the mechanism of injury and symptoms. Additionally, any child with a head injury, multi-system trauma, or conditions predisposing them to cervical instability should be considered to have a cervical spine injury until proven otherwise.2 It is important to note potential predisposing conditions that may increase the risk of cervical spine injury. These include Down syndrome, Ehlers-Danlos syndrome, Marfan syndrome, juvenile idiopathic arthritis, juvenile ankylosing spondylitis, and osteogenesis imperfecta, among others.1
Upper cervical spine injuries (C1-C4) are almost twice as common as lower cervical spine injuries (C5-C7). This is because children have a large head size relative to their body, which puts them at risk for the “fulcrum effect.” The fulcrum in very young children is at the C2/C3 level. As the body size increases with age, the fulcrum moves down, leading to more distal locations of fractures in older children.2
It also is important to note that spinal injury in young children can be fatal, even with minimal structural damage. This is because of the increased flexibility of the pediatric spine secondary to greater ligamentous laxity, poor musculature, open ossification centers, and physiologic wedging of immature vertebral bodies.2 The pediatric spinal column can be distracted up to 5 cm without any structural injury, whereas the spinal cord cannot. This difference puts children at risk for spinal cord injury without radiographic abnormality (SCIWORA).2
Anatomic Differences
There are many differences between pediatric and adult cervical spine anatomy. Knowing this anatomy is of the utmost importance when evaluating and treating spinal pathology in pediatric patients. The most notable difference in the pediatric cervical spine is the presence of physes (growth plates). Normal variation of the physis and incomplete ossification of synchondroses and apophyses can be falsely identified as a fracture.4
When distinguishing a fracture from a physis, a physis typically has smooth edges and is present in a predictable location, such as the spinous processes or neural arches. A normal occurring physis will be smooth with a regular structure along with subchondral sclerosis on either side. The physeal line on imaging will be well-demarcated and symmetric. In contrast, an acute fracture will be irregular and not have defined sclerotic margins. Additionally, fractures will occur in atypical areas from physes, making the knowledge of normal anatomy critical.5
The upper cervical spine in pediatric patients is specifically unique because of the ossification centers. The C1 vertebra (atlas) has three separate ossification centers: one in the anterior vertebral arch and two in the lateral masses. These fuse around 7 years of age. Lack of union or delayed union in the ossification centers can be confused for a fracture.6 The C2 vertebra (axis) uniquely has a total of five primary ossification centers. These include a central ossification center in the C2 body, two in the posterior neural arch, and two in the odontoid (dens). Around the age of 6-7 years, the subdental synchondrosis at the junction of the dens and C2 body will fuse, although this may persist until the age of 11 years. The normal subdental synchondrosis can be distinguished from an acute fracture because the synchondrosis will sit below the C1-C2 facet joints.6 The secondary ossification centers of the dens, more cranially, form initially between the ages of 3 to 7 years. They then typically will fuse at 12 years of age. This will be discussed later when referring to specific fracture patterns of the dens.
In contrast to the upper cervical spine, the subaxial cervical spine typically will develop in a more predictable developmental pattern. The four ossification centers in each vertebra include one in the body, two in the lateral masses, and an additional ossification center in the posterior arch. The neural arch typically fuses between 2 and 3 years of age, with the body fusing in the midline around 3 years of age. The neural arches then will fuse to the body at the lateral masses between the ages of 3 and 6 years. Secondary ossification centers will be present both above and below the vertebral bodies.6
Normal pediatric vertebral bodies are ovoid in appearance on lateral imaging. They will begin to take on a more regular shape with age. Along with the ovoid appearance, pediatric vertebral bodies can have physiologic wedging, or a compressed appearance. Anterior wedging is most prominent in the upper cervical spine at C3 and occurs in the anterior and superior edge.7 A normal vertebral body in a child may have wedging up to 3 mm.8,9 This is thought to be partially caused by hypermobility in younger patients.
Physical Exam
Any child with a suspected cervical spine injury should be immobilized prior to transport. Interestingly, because a child has a relatively larger head, a specialized backboard consisting of a bump beneath the upper thoracic spine or a cutout in the board for the head should be used to prevent neck flexion.10 The physical exam is extremely important when evaluating for pediatric cervical spine injuries. For an adequate exam, the patient must be awake, alert, and cooperative. The Glasgow Coma Scale (GCS) score should be calculated, and the examination should focus on vital signs, a neck exam, and a neurologic evaluation. Primarily, vital signs are important to assess because upper cervical spine injuries can present with hypotension or apnea and hypoventilation caused by loss of diaphragmatic control, since C3-C5 innervate the diaphragm.11
The cervical spine should be held in place by one person while another person removes the cervical collar and gently palpates the posterior midline of the neck, then lateral to midline on both sides.
Midline tenderness to palpation is the most common physical exam finding in cervical spine injuries. The patient should be re-immobilized in a cervical collar if there is pain with palpation. If there is no tenderness to palpation, range of motion can be assessed. Additionally, a full neurologic exam, including evaluation of the patient’s strength, sensation, reflexes, and rectal tone, should be performed.12 Imaging should be obtained immediately if a child has neck pain or midline posterior neck tenderness, decreased range of motion, muscle spasms, altered mental status, or focal neurologic findings.12 However, it is important to remember that a significant portion of pediatric cervical spine injuries may be asymptomatic.1
Table 1 summarizes the various physical examinations to perform and the findings that would signify possible cervical spine injury.
Table 1. Physical Examination Findings Indicating Cervical Spine Injuries |
|
| Physical Examination | Findings that Signify Possible Cervical Spine Injury |
Vitals/Glasgow Coma Scale |
|
Neck examination |
|
Neurologic examination |
|
Clinical Clearance
Unfortunately, clinical decision-making tools, such as the Canadian C-spine Rule and the National Emergency X-radiography Utilization Study (NEXUS) criteria, have not been well studied in the pediatric population. For example, the Canadian C-spine Rule included no patients younger than 16 years of age. The NEXUS criteria only included 2.5% of patients 8 years of age or younger, and among patients with a cervical spine injury, only 1.3% were 8 years of age or younger.13
In 2019, a multidisciplinary expert panel came up with a comprehensive consensus statement and algorithm to clear the cervical spine in children after trauma.14 This panel was based on a case-controlled study conducted by the Pediatric Emergency Care Applied Research Network, which identified significant risk factors and physical exam findings in 540 children from 0-15 years of age with cervical spine injuries.11
In developing this algorithm, the panel emphasized the thoughtful use of CT scans to reduce the risk of radiation in children while also balancing the risks of missing a cervical spine injury. The algorithm is determined based on initial GCS scores. If the GCS is 14 or 15, clinical clearance is recommended with the goal of minimizing radiation exposure. If the GCS is 9-13 and is likely to improve within 72 hours, clinical gestalt and judicious use of CT is recommended. Lastly, if the GCS is ≤ 8, a CT scan is recommended. This algorithm was meant to serve as a foundation for institutionalized protocols regarding cervical spine clearance.14 There currently is no validated clinical tool to clear the pediatric cervical spine.
Diagnostic Considerations
It is important for the emergency physician to consider radiation exposure when deciding on imaging to evaluate for pediatric cervical spine injuries. CT scans in pediatric patients likely result in significantly increased risk of malignancy over CT scans in adults. This is because children have more years to develop cancer than adults and they are more radiosensitive.15 Thus, conventional X-rays are the most frequently used initial imaging modality if a very high suspicion for cervical spine injury is not present.
The recommended radiographic series includes frontal, lateral, and open-mouth odontoid views. Flexion and extension radiographs are not recommended in the acute setting.16 CT scans typically are reserved for patients who have experienced polytrauma, are obtunded, or are at a high risk because of the mechanism of injury or individual risk factors. In high-risk children, a negative CT scan does not fully exclude injury. These children may need magnetic resonance imaging (MRI). MRI is the most sensitive and specific imaging modality in acute pediatric spine injury.15 It identifies soft tissue and ligamentous injuries very well, which are poorly visualized on CT scan. However, providers must keep in mind that MRI is costly and often requires sedation. Table 2 summarizes the reasons to consider specific imaging modalities.
Table 2. Imaging Modality Criteria for Cervical Spine Injuries |
|
| Imaging Modality | Reason for Selection |
None |
|
X-ray |
|
Computed tomography (CT) |
|
Magnetic resonance imaging |
|
Adapted from McAllister AS, Nagaraj U, Radhakrishnan R. Emergent imaging of pediatric cervical spine trauma. Radiographics 2019;39:1126-1142. |
|
Cervical Spine Injuries
There are numerous types of injuries that can affect the pediatric cervical spine. Specifically, there are unique fractures and instability patterns that occur in children. This article will focus on injuries that are present in pediatric patients and in which diagnosis can be difficult, given the anatomic and physiologic differences in younger patients. Fracture dislocations, such as a C1 Jefferson fracture, C2 hangman’s fractures, and subaxial fracture dislocations, are diagnosed and treated in a manner similar to adults. Therefore, they will not be discussed in this article.
Atlanto-occipital Dissociation
Possibly the most feared and devastating injuries in pediatric patients are those of the upper cervical spine, specifically in the atlanto-occipital joints and the atlanto-axial joints. Atlanto-occipital injures, including atlanto-occipital dissociation (AOD), occur because of instability at the occipitocervical (OC) junction. This is a spectrum of injuries that ranges from partial to complete disruption of the tectorial membrane (the most cranial extension of the posterior longitudinal ligament) and the apical and bilateral alar ligaments, which connect the basilar skull to the cervical spine.17
Historically, AOD was considered non-survivable because it was frequently associated with cardiopulmonary arrest, neurogenic shock, or severe neurologic impairment secondary to upper cervical spinal cord or brainstem injury. However, there is an increasing incidence of AOD caused by improved automotive restraints and first-responder management, which allows these patients to make it to the trauma bay alive. Additionally, improved advanced imaging and high clinical suspicion of the injury may result in improved diagnosis of AOD.18 Typically, initial AOD diagnosis is made on lateral X-ray or CT scan of the cervical spine.
When assessing for AOD, there are many measurements and ratios that have been developed to aid diagnosis. However, there is no single method that is perfectly sensitive and specific for the diagnosis. Typically, evaluation and diagnosis are made by a combination of multiple measurements or ratios, aided by cross-sectional imaging. Lateral cervical spine X-ray measurements are most useful for triggering the use of advanced imaging.
The basion-dens interval (BDI) and the interspinous ratio have been shown to have the highest sensitivity and specificity for detecting AOD and triggering the need for MRI.17 The BDI is measured from the tip of the basion (the anterior aspect of the foramen magnum) to the tip of the dens on lateral cervical spine X-ray. (See Figure 1.) This was described initially by Wholey as a BDI < 10 mm being considered normal.19 The C1/C2:C2/C3 interspinous ratio is calculated by measuring the interspinous distance of C1/C2 divided by C2/C3 interspinous distance. As described by Sun, a ratio of > 2.5 is diagnostic of a tectorial membrane rupture.20
Figure 1. Demonstration of the Basion-Dens Interval Measurement |
 |
Courtesy of Joy Hallmark, MD. |
Additionally, the evaluation of Wackenheim’s clivus line can be used, although this is less sensitive and specific than the previously mentioned measurements. The clivus is a bony portion of the cranium at the central base of the skull. A line is drawn from the caudal extension of the dorsal inferior clivus to the dens. If the line sits above the tip of the dens, then there should be concern for AOD.21 Of note, this line can be greatly affected by the flexion or extension at the OC junction in an uninjured spine. Similarly, the Powers ratio can be used similarly to the Wackenheim’s line with decreased sensitivity and specificity compared to the BDI and interspinous ratio.
The Powers ratio is calculated as the distance of the basion to C1 divided by the distance of the opisthion (posterior aspect of the foramen magnum) to the posterior aspect of the C1 arch. A Powers ratio of < 1 is considered normal, and an increasing ratio is concerning. However, the Powers ratio is only 37.5% sensitive.6
Cross-sectional imaging with CT or MRI is invaluable in the diagnosis of AOD. A CT scan is useful when evaluating the width of the atlanto-occipital (AO) joint space. The AO joint space is measured bilaterally at four different points in both the coronal and sagittal planes. These distances are averaged. An average AO distance of > 4 mm is considered abnormal and is 100% sensitive and specific for AOD.22,23
Atlantoaxial Injuries
When considering the pediatric upper cervical spine, the atlantoaxial (AA) joint is also at risk of injury. AA dislocation or subluxation refers to an imperfect alignment of C1 on C2.24 Dislocation or subluxation of the AA joint can occur because of high energy trauma with frank disruption of the tectorial membrane. In high energy trauma events, there always is concern for neurologic injury.
In contrast, a lower energy trauma can lead to a rotatory subluxation with or without anterior translation.25 A muscle spasm can occur in the setting of inflammation, low energy trauma, or an infection of the anterior spine and pharynx.26 In some cases, AA subluxation can occur without obvious injury. Grisel syndrome refers to a spontaneous and atraumatic rotatory subluxation that presents as torticollis. This typically occurs in predisposed children with genetic disorders, most commonly Down syndrome.24
In the setting of trauma, AA instability can be evaluated on lateral cervical spine films, like AOD. The atlas-dens interval (ADI) is measured from the posterior aspect of the anterior ring of C1 to the anterior aspect of the dens. In a pediatric patient, a normal ADI should be 5 mm or less (as opposed to ≤ 3 mm that is considered normal in adults). If the ADI is < 5 mm, it is likely the tectorial membrane is intact. If the ADI is > 5mm in flexion or neutral, or > 4 mm in extension, an MRI should be ordered to further evaluate the ligamentous stabilizing structures.
As mentioned, a rotatory AA subluxation can occur with minimal instability or even spontaneously, such as Grisel syndrome. This presents with torticollis with an ipsilateral rotation and a contralateral tilt of the head in relation to the C1 lateral mass.24 The chin is rotated to the side opposite of the facet subluxation (for example, a left-sided facet subluxation will have the chin rotated to the right), with a spastic sternocleidomastoid (SCM) muscle occurring on the same side as the chin. In this case, a left-sided facet subluxation will have a spastic right SCM as a compensation to reduce further subluxation. With AA rotatory subluxation, the C1-C2 subluxation is the primary issue, with the SCM spasm being secondary.
This contrasts with congenital muscular torticollis where the SCM spasm occurs contralaterally to the side that the chin turns. Congenital muscular torticollis is a primary driving force with a secondary C1-C2 rotation.26 In both cases, the child presents with reduced cervical rotation.25
In the setting of atraumatic or minimally traumatic injuries, anterior-posterior (AP) and open mouth X-ray views should be obtained. However, such injuries are best evaluated with a CT scan for maximum sensitivity where there is a fixed rotation of C1 on C2 on dynamic CT scan with both neutral and maximal left and right rotation of the cervical spine.25 Dynamic CT imaging should be obtained only when a patient presents with torticollis in an atraumatic setting. Practitioners should avoid dynamic CT imaging with cervical rotation in the setting of traumatic AA instability.
Odontoid Fractures vs. Os Odontoideum
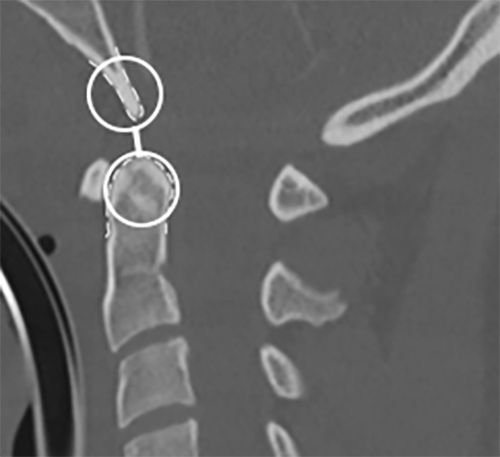
An os odontoideum (OO) is another mimicker of spinal trauma. An OO represents a congenital anomaly of the C2 vertebra. (See Figure 2.) The OO is an independent bony ossicle of variable size and shape that is a separate entity from the odontoid process.27 The OO can be either orthotopic (sitting in normal position above the odontoid process) or a dystopic os (fused to the basion).
Figure 2. Demonstration of an Os Odontoideum on Sagittal Cervical Spine Computed Tomography |
 |
The arrow points to an identified os odontoideum. Courtesy of Joy Hallmark, MD. |
There is significant debate regarding the etiology of an OO. Whether this represents a congenital anomaly or the sequelae of a remote trauma has yet to be determined.28 An OO can be distinguished from an acute fracture based on imaging, including lateral cervical spine X-ray and CT, by having a smooth, regular border and in the typical location described. Since this may result from a nonunion of the secondary ossification center at the tip of the odontoid, the location can help distinguish an OO from acute fracture.29
Once the diagnosis of an OO is made, a thorough neurologic exam is vital. Despite possibly being congenital in nature, OO can become symptomatic even with minor or no history of trauma. Symptoms frequently present in late adolescence with neck pain, shoulder pain, and headaches. Even severe symptoms, such as myelopathy and those of vertebrobasilar ischemia, have been reported. This is hypothesized to be caused by slow progression of AA instability.27
In contrast, an acute odontoid fracture typically occurs in high-energy mechanisms in younger patients. These fractures occur because of cervical hyperflexion or hyperextension in the setting of blunt trauma.
In very young patients (younger than 10 years of age), the fracture typically occurs at the site of the basilar synchondrosis. Odontoid fractures are the most common fractures of the atlas and account for nearly 15% of all cervical fractures.29 Similar to evaluation of an OO, a detailed neurologic exam is vital when evaluating an odontoid fracture. (See Figure 3.)
Figure 3. Odontoid (Dens) Fracture |
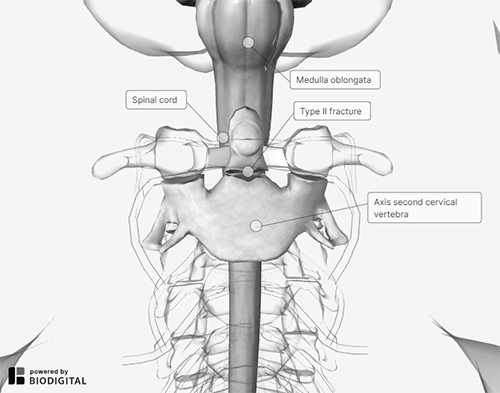 |
Courtesy of BioDigital. |
Ligamentous Injuries
Ligamentous injuries to the cervical spine include those of the atlanto-occipital joint, atlantoaxial joint, and the subaxial spine. These can involve the intervertebral disc, the facet joints, and the posterior ligaments. A true injury through these structures can lead to instability, subluxation, or frank dislocation. As with other pathologies in the pediatric cervical spine, normal anatomy must be distinguished from true injury.
Pseudosubluxation
When considering ligamentous injuries and instability, an anatomic variant that must be recognized in the pediatric cervical spine is pseudosubluxation. This normal variant can be mistaken for an unstable cervical spine injury if seen on imaging following a trauma.
Pseudosubluxation most commonly occurs at the atlantoaxial joint, but it also can occur in the subaxial spine.6 The C2-C3 and the C3-C4 joints have a normal apparent displacement in the pediatric spine. However, providers should be aware that, on lateral flexion extension films, the C2-C3 joint can have an apparent subluxation in up to 50% of children younger than 8 years of age, even in asymptomatic patients without injury.6 (See Figure 4.) This typically is seen along the anterior vertebral body. This also can occur to a lesser extent at the C3-C4 joint.
Figure 4. Demonstration of Pseudosubluxation on Lateral Cervical Spine X-Ray |
 |
The dashed line drawn above indicates a normal posterior cervical line. Courtesy of Joy Hallmark, MD. |
The posterior cervical line is used to distinguish pseudosubluxation from an unstable injury. The posterior cervical line runs along the anterior aspect of the spinous processes on lateral cervical spine films. This line should be within 1 mm of each spinous process on flexion and extension. The posterior cervical line should be smooth and continuous without a sudden step-off or break noted.
In pseudosubluxation, the posterior cervical line will be intact, even if the anterior cerebral bodies have subluxation or step-off.6 In contrast, if the posterior cervical line falls > 2 mm away from the spinous processes, then a true injury likely is present. This happens most commonly in the setting of traumatic spondylolisthesis, also known as a “hangman’s” bilateral pars fracture of C2.30 While pseudosubluxation occurs on lateral cervical spine imaging, a similar physiologic finding can be found on AP/open-mouth odontoid views.
A “pseudo-Jefferson burst fracture” is when there is a physiologic spread of the atlas on the axis. The spread is considered within normal limits if there is ≤ 6 mm of combined displacement of the lateral masses relative to the C2 facets.31 The Rule of Spence and Heller states that a spread of < 7-8 mm of the C1 lateral masses indicates an intact transverse atlantal ligament. In contrast, if there is fracture and > 8 mm of combined spread, then an unstable transverse ligament rupture should be suspected.32
Other Anatomic Variants on Imaging
Lastly, other normal variants must be distinguished from pathology. First is the loss of cervical lordosis on lateral films. This can be seen in pediatric patients up to 16 years of age.31,33 Interspinous distance also can be irregular at contiguous levels. When evaluating for injury, a single interspinous distance in the subaxial cervical spine should not be greater than 1.5 times that of the level above or below it.33
Increased spacing should prompt MRI imaging to evaluate the posterior ligamentous structures. Specifically, the C1-C2 joint can have physiologic widening with flexion. This is in part because of the tight ligamentous structures between the occiput and C1. C1-C2 AA instability should be evaluated as mentioned earlier if there is suspicion for injury. Finally, soft tissue swelling on lateral films can be a clue of acute injury.
In the setting of trauma, edema and hemorrhage can lead to soft tissue swelling anterior to the pediatric cervical spine. This soft tissue thickness is considered normal if it is < 6 mm at the C3 level. This can be altered based on normal respirations, so repeat lateral cervical spine films with inspiration and expiration or an MRI can be obtained if there is concern for injury.7 In summary, there are numerous unique findings in the setting of cervical spine injury in the pediatric population. Knowing the normal anatomy, physiologic variants, and unique injury patterns can aid in the diagnosis of a trauma.
SCIWORA
SCIWORA was first described by Pang et al in 1982 and describes an acute spinal cord injury resulting in neurologic deficits without evidence of bony injury or misalignment on radiographs or CT scans.34 This phenomenon is caused by the hypermobility of the pediatric cervical spine, and, thus, occurs mainly in the pediatric population. Most SCIWORA injuries occur in the cervical spine, but they also can occur in the thoracic spine.
Interestingly, they can have delayed onset of signs and symptoms, so repeating a thorough neurological exam and MRI should be considered. This should be done about 48-72 hours after the initial work-up. SCIWORA usually results after severe trauma and is the consequence of flexion, extension, and distraction injuries.34 These injuries can lead to spinal cord hemorrhage or edema, culminating with neurologic deficits.
Patients with major hemorrhage seen on MRI typically will have long-term impairment, whereas those with no findings on MRI usually make a full recovery.35 It is imperative to identify and stabilize these injuries early to provide the best long-term outcome. It also is important to remember that minor trauma after an initial SCIWORA can lead to recurrent and worsening symptoms because of increased vulnerability of the injured spinal cord.36
Treatment of SCIWORA typically requires prolonged immobilization with a cervical collar (eight to 12 weeks).36 Steroid therapy should not be considered; it has not been proven to be beneficial.36
Management
Initial immobilization during evaluation of a pediatric cervical spine trauma is always vital during workup and imaging and should be pursued in the prehospital setting or in the emergency department. For all children with midline cervical spine tenderness or neurologic abnormalities, a neurosurgeon or orthopedic spine surgeon should be consulted. If these services are unavailable, the child should be transferred immediately to a tertiary care center with these capabilities.
Specific treatment of pediatric cervical spine injuries is beyond the scope of this article. In brief, normal anatomic variants, such as pseudosubluxation or an asymptomatic os odontoideum, can be managed with simple observation and outpatient follow-up. Spine injuries, such as stable odontoid or stable subaxial cervical spine fractures, can be treated with rigid collar immobilization.
Surgical management, in the form of halo vest immobilization or cervical fusion, is indicated for unstable injuries, irreducible fractures/dislocations, or worsening neurological deficits.38 It is important to account for the potential growth of the pediatric spine, since surgical fixation and fusion can limit future growth and lead to deformities.39
Conclusion
Cervical spine injury is rare in children but can have devastating consequences. Differences from adults in terms of anatomy, biomechanics, injury patterns, and imaging findings must be considered when evaluating these patients.
Emergency physicians should have a high clinical suspicion for these injuries in the pediatric trauma patient, and initial management should focus on prompt immobilization of the cervical spine to prevent further injury, a thorough physical exam, and appropriate imaging. Spine surgeon consultation should follow initial management.
REFERENCES
- Nagler J, Farrell CA, Auerbach M, et al. Trauma. In: Shah BR, Mahajan P, Amodio J, Lucchesi M, eds. Atlas of Pediatric Emergency Medicine. 3rd edition. McGraw Hill;2019:947-1044.
- Gopinathan NR, Viswanathan VK, Crawford AH. Cervical spine evaluation in pediatric trauma: A review and an update of current concepts. Indian J Orthop 2018;52:489-500.
- Babcock L, Olsen CS, Jaffe DM, et al; Cervical Spine Study Group for the Pediatric Emergency Care Applied Research Network (PECARN). Cervical spine injuries in children associated with sports and recreational activities. Pediatr Emerg Care 2018;34:677-686.
- Baerg J, Thirumoorthi A, Hazboun R, et al. Cervical spine injuries in young children: Pattern and outcomes in accidental versus inflicted trauma. J Surg Res 2017;219:366-373.
- Pang D, Thompson DN. Embryology and bony malformations of the craniovertebral junction. Childs Nerv Syst 2011;27:523-564.
- Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: Normal anatomy, variants, and trauma. Radiographics 2003;23:539-560.
- Swischuk LE, Swischuk PN, John SD. Wedging of C-3 in infants and children: Usually a normal finding and not a fracture. Radiology 1993;188:523-526.
- Cattell HS, Filtzer DL. Pseudosubluxation and other normal variations in the cervical spine in children. J Bone Joint Surg Am 1965;47:1295-1309.
- Shaw M, Burnett H, Wilson A, Chan O. Pseudosubluxation of C2 on C3 in polytraumatized children: Prevalence and significance. Clin Radiol 1999;54:377-380.
- Shah M, Herman MJ, Eberson C, Anderson JT. Pediatric and adolescent cervical spine trauma. In: Hedequist D, Shah S, Yaszay B, eds. The Management of Disorders of the Child’s Cervical Spine. Springer;2018:87-120.
- Leonard JC, Kuppermann N, Olsen C, et al. Factors associated with cervical spine injury in children after blunt trauma. Ann Emerg Med 2011;58:145-155.
- Copley PC, Tilliridou V, Kirby A, et al. Management of cervical spine trauma in children. Eur J Trauma Emerg Surg 2019;45:777-789.
- Hoffman JR, Wolfson AB, Todd K, Mower WR. Selective cervical spine radiography in blunt trauma: Methodology of the National Emergency X-Radiography Utilization Study (NEXUS). Ann Emerg Med 1998;32:461-469.
- Herman MJ, Brown KO, Sponseller PD, et al. Pediatric cervical spine clearance: A consensus statement and algorithm from the Pediatric Cervical Spine Clearance Working Group. J Bone Joint Surg Am 2019;101:e1.
- Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176:289-296.
- McAllister AS, Nagaraj U, Radhakrishnan R. Emergent imaging of pediatric cervical spine trauma. Radiographics 2019;39:1126-1142.
- du Plessis J-P, Dix-Peek S, Hoffman EB, et al. Pediatric atlanto-occipital dissociation: Radiographic findings and clinical outcome. Evid Based Spine Care J 2012;3:19-26.
- Brown RL, Brunn MA, Garcia VF. Cervical spine injuries in children: A review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg 2011;36:1107-1114.
- Wholey MH, Bruwer AJ, Barker HL. The lateral roentgenogram of the neck: With comments on the atlanto-odontoid-basion relationship. Radiology 1958;71:350-356.
- Sun P, Poffenbarger J, Durham S, Zimmerman RA. Spectrum of occipitoatlantoaxial injury in young children. J Neurosurg 2000;93(Suppl 1):28-39.
- Wackenheim A. Angles and Lines of Measurement in the Craniovertebral Region. Springer-Verlag; 1974.
- Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation—part 2: The clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery 2007;61:995-1015; discussion 1015.
- Pang D, Nemzek WR, Zovickian J: Atlanto-occipital dislocation: Part 1—normal occipital condyle-C1 interval in 89 children. Neurosurgery 2007;61:514-521; discussion 521.
- Ghanem I, El Hage S, Rachkidi R, et al. Pediatric cervical spine instability. J Child Orthop 2008;2:71-84.
- Mazzola CA, Christie C, Snee IA, Iqbal H. Atlantoaxial subluxation in the pediatric patient: Case series and literature review. Journal of Neuroscience and Neurological Disorders 2020;4:69-74.
- Park S-H, Park S-H, Lee S-H. Grisel syndrome: Pathophysiological evidence from magnetic resonance imaging findings. Ann Rehabil Med 2013;37:713-716.
- Visocchi M, Fernandez E, Ciampini A, Di Rocco C. Reducible and irreducible os odontoideum in childhood treated with posterior wiring, instrumentation and fusion. Past or present? Acta Neurochir 2009;151:1265-1274.
- Fielding JW, Hensinger RN, Hawkins RJ. Os odontoideum. J Bone Joint Surg Am 1980;62:376-383.
- Jumah F, Alkhdour S, Mansour S, et al. Os Odontoideum: A comprehensive clinical and surgical review. Cureus 2017;9:e1551.
- Swischuk LE. The spine and the spinal cord, 4th ed. In: Emergency Imaging of the Acutely Ill or Injured Child. Lippincott Williams & Wilkins;2000:532-587G.
- Suss RA, Zimmerman RD, Leeds NE. Pseudospread of the atlas: False sign of Jefferson. AJR Am J Roentgenol 1983;140:1079-1082.
- Roche C, Carty H. Spinal trauma in children. Pediatr Radiol 2001;31:677-700.
- Heller JG, Viroslav S, Hudson T. Jefferson fractures: The role of magnification artifact in assessing transverse ligament integrity. J Spinal Disord 1993;6:392-396.
- Hall DE, Boydston W. Pediatric neck injuries. Pediatr Rev 1999;20:13-19.
- Pang D, Wilberger Jr. JE. Spinal cord injury without radiographic abnormalities in children. J Neurosurg 1982;57:114-129.
- Pang D. Spinal cord injury without radiographic abnormality in children, 2 decades later. Neurosurgery 2004;55:1325-1342; discussion 1342-1343.
- Baker C, Kadish H, Schunk JE. Evaluation of pediatric cervical spine injuries. Am J Emerg Med 1999;17:230-234.
- Kreykes NS, Letton Jr. RW. Current issues in the diagnosis of pediatric cervical spine injury. Semin Pediatr Surg 2010;19:257-264.
- Mortazavi M, Gore PA, Chang S, et al. Pediatric cervical spine injuries: A comprehensive review. Childs Nerv Syst 2011;27:705-717.
