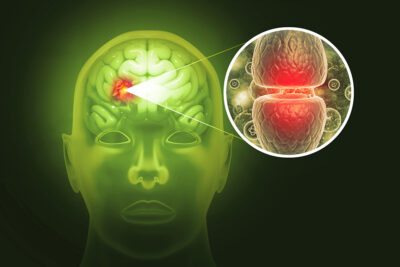
Frontotemporal lobar degeneration commonly occurs with motor neuron disease and has similar cytoplasmic neuronal aggregates of TAR deoxyribonucleic acid-binding protein 43 (TDP-43) in the brain as well as the spinal cord.
ABSTRACT & COMMENTARY
Clinicopathological Correlation in Motor Neuron Disease and Frontotemporal Degeneration
October 1, 2024
