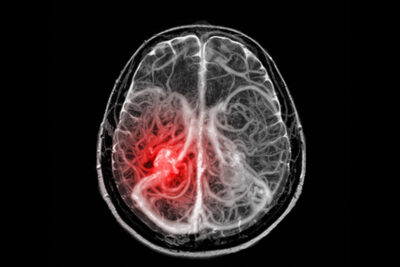
This randomized trial from China demonstrates a dramatic benefit from endovascular thrombectomy in patients with acute basilar artery occlusion. This benefit was sustained and improved at one year compared to 90 days.
ABSTRACT & COMMENTARY
Thrombectomy for Basilar Artery Occlusion
October 1, 2024
